
![]()
icture a beautiful newborn so fragile that stroking her irresistible
pink cheek leaves a trail of blisters that turn into raw, oozing
wounds. Imagine an active baby with the knees of his padded cotton
pants soaked in blood from the normal act of crawling. Or a teenager
with stumps for hands, the affected fingers long gone.
This is the nightmare of life with epidermolysis bullosa (EB), an inherited disease that affects 100,000 children and adults in the United States. People born with EB lack anchors that hold the layers of their skin together. As a consequence, any activity that rubs or causes pressure produces a painful sore akin to a second-degree burn. Many forms of EB are lethal in the first weeks or months of life. Most are mutilating over time. Infection is a serious, ongoing concern.
As if the diagnosis is not heartbreaking enough, no treatment for EB has been effective. Parents have coped by protecting the child's skin with padded clothing as best they could and applying antibiotic ointment to the inevitable wounds that occurred. But because of extensive clinical research done by University of Miami dermatologists, the future for these patients looks, well, rosier, as a baby's cheek should.
EB was one of the reasons Lawrence A. Schachner, M.D., director of pediatric dermatology, chose to enter his specialty field. As an intern, he was intensely frustrated by futile efforts to treat the disease, and made up his mind to do whatever he could to help these children. Over the years, he went about it scientifically, studying new products as they came along.
"I saw many children and spoke and published many times, usually on treatment failure, trying to de-myth the fact that some new wonder drug was going to do the trick," he says.
So as he watched his colleagues in the University of Miami Department of Dermatology and Cutaneous Surgery conduct clinical trials on adults with hard-to-heal leg ulcers using a bioengineered skin called Apligraf, he silently wondered if the product might be worth trying on EB.
"I thought if I ever had a severe enough child and a strong enough family, I would be comfortable trying a treatment that not only had never been used for EB, but had never been used on a baby," he remembers. "But it had to be the right family that could understand all the nuances."
The right family was the Camerons of Boca Raton, Florida. Randy and Lorraine Cameron's second child, Tori, was born in November 1998 with EB blisters covering 70 percent of her body. Due to the seriousness of her disease, she was immediately transferred to University of Miami/Jackson Children's Hospital at the Holtz Center for Child and Maternal Health, where the physicians routinely treat severely ill children. It was the opportunity Dr. Schachner had been waiting for. Tori was so young that her naive immune system might better accept the Apligraf cells.
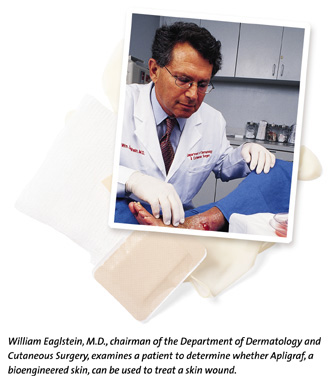
With the Camerons' full consent, Dr. Schachner--in collaboration with Anna Falabella, M.D., and William Eaglstein, M.D., members of the Department of Dermatology and Cutaneous Surgery's Wound Healing Team--ordered a delivery of freshly grown Apligraf from its developer. When it arrived, they lifted patches of this living skin-equivalent from their dishes of pink gelatin, laid them on the one-week-old baby's wounds, and wrapped her in gauze. Four days later they carefully removed Tori's bandages. Where they had placed Apligraf, her skin was pink, healthier, and blister-free.
For Dr. Schachner, it was the first major break in 25 years of searching for a solution to this devastating disease. Excited, but cautious about claiming success with a single patient, the three collaborators arranged a clinical trial involving 15 more children. In similar fashion, most of their wounds disappeared in only four days, leaving grafts that blended beautifully into the surrounding skin.
"It was one of the best days I've had as a doctor," he says with a smile.
![]() pligraf
may seem like a miracle, but success did not come overnight.
Pre-clinical research and the testing of medications, techniques,
and products like Apligraf to determine their effectiveness are
a time-consuming, ongoing process in the Department of Dermatology
and Cutaneous Surgery, where the faculty and residents seek answers
to challenging medical conditions by conducting more than 30
clinical trials at a time.
pligraf
may seem like a miracle, but success did not come overnight.
Pre-clinical research and the testing of medications, techniques,
and products like Apligraf to determine their effectiveness are
a time-consuming, ongoing process in the Department of Dermatology
and Cutaneous Surgery, where the faculty and residents seek answers
to challenging medical conditions by conducting more than 30
clinical trials at a time.
Apligraf first came to the attention of Dr. Eaglstein, the department's chairman, in the early 1990s. A specialist in wound care, he was on the lookout for ways that bioengineered tissue might be used to benefit patients with non-healing wounds. Over the years, he had worked with many types of laboratory-grown skin, and had even pioneered wound coverings that kept wounds moist, improved healing time, and reduced patient discomfort. But no equivalent of living human skin had ever been found.
When Dr. Eaglstein read about Apligraf, he was intrigued. Created
as a potential treatment of chronic leg ulcers, Apligraf is a
combination of bovine (cow) collagen mixed with human keratinocytes,
which are epidermal cells that make proteins. The resulting material
is combined with human fibroblasts, dermal cells that make connective
tissue, which are obtained from circumcised foreskins. It is
the world's first bioengineered skin with these two layers: an
epidermis, epidermal cells that from a protective layer to ward
off infections, and a dermis, dermal cells that provide strength
and elasticity. Dr. Eaglstein contacted the developer and arranged
clinical trials on the product.
By 1995, Apligraf's value in treating chronic wounds was clear. Covering the wound with Apligraf made the patient's own skin grow faster underneath. Encouraged by the results, he convinced the developer to allow a clinical trial on acute wounds, such as donor sites, wounds created when a patient's healthy skin is scraped off for use as a skin graft to cover a leg ulcer. Two scrapes were made on each patient's skin and covered with Apligraf, polyurethane film, or the patient's own skin. It was the first study ever done comparing a tissue-engineered skin with real skin, and the results were even better than for chronic wounds.
"We found that Apligraf was almost like the patient's own skin. Both healed faster than the polyurethane film, and the cosmetic results were better," says Dr. Eaglstein. "It was clear that using a tissue-engineered skin product could spare patients the second wound of using their own skin, with its attendant discomfort and risks."
Another trial followed in which Apligraf was tried on other types of acute wounds, including places where cancers had been removed. As in the donor site trials, two months after application the Apligraf sites were pink and healthy. In many patients, the graft blended so well into the surrounding skin that it could no longer be detected. No signs of infection or overt rejection were seen. As a result of these accumulated clinical trials, the Food and Drug Administration approved Apligraf for use in adults.
Since the approval, Dr. Falabella has been applying Apligraf to patients with problematic wounds that heal slowly. Her patients have responded well, and currently she's using the product to treat patients with venous ulcers.
"We've had great success with this product," Dr. Falabella says. "As for Tori, I am happy that we were able to help her graduate from that critical period of time when any infection was a threat to her life because of her open sores."
![]() hat no
one knows is whether Apligraf is absorbed, integrated, or replaced
by new skin. Ongoing DNA testing of patch sites will reveal the
healing process over time. Meanwhile, Dr. Eaglstein considers
Apligraf a treatment, not merely a wound covering.
hat no
one knows is whether Apligraf is absorbed, integrated, or replaced
by new skin. Ongoing DNA testing of patch sites will reveal the
healing process over time. Meanwhile, Dr. Eaglstein considers
Apligraf a treatment, not merely a wound covering.
"Apligraf is like a factory that makes chemicals for healing. We have reason to believe it heals by stimulating the host tissue," Dr. Eaglstein explains. "With chronic ulcers, we may put Apligraf on the wound every week for a while. It makes a lot of chemicals that encourage the skin to heal. It's like giving a dose of skin."
For children with EB, a chemical factory is exactly what the doctor ordered. Patients like Tori lack certain keratinocyte proteins in their skin, and Apligraf's success may be partly due to its ability to deliver these proteins, Dr. Schachner explains. While he must wait and see if the positive effect will withstand the test of time, the short-term effect surpassed his wildest hopes.
"We asked the parents which sites were the worst, the most painful, and these were the sites we grafted," Dr. Schachner says. "All the children had some benefit, and some have had complete benefit. One child had a three-inch, one-year-old chronic ulcer on the back of her neck that oozed and hurt all the time. We grafted the wound, and four days later, the child had no bleeding and no pain in that area. That's what I call-at least over the short haul-a complete success story."
Apligraf is not the end of the line for Dr. Schachner, but merely the beginning. Further clinical trials are now needed to address many questions that must be answered before the product can be approved for use in this disease. He expects the next step to be a controlled comparison study where side-by-side, freshly created blisters are treated with Apligraf and a more conventional therapy.
The success of this bioengineered tissue has opened up a world of possibilities. Dr. Schachner's mind has already leaped ahead to the ways an Apligraf-like product might help children with EB blisters inside the body.
"I believe if you can make a living skin-equivalent, you can make a bioengineered mucosa. It would be a big challenge for a biotech company, but it's very exciting," he says enthusiastically.
Meanwhile, he looks forward to seeing progress in the lucky 16 who have already benefited from their new skin. "I'm privileged to be part of an exciting academic medical center where research is encouraged and fostered," he says. "It's almost a new millennium, and we are going to make new millennium things happen."