 |
 |
|
 |
||
A FAILURE TO COMMUNICATE
![]()
n August 14, 2003, a breakdown in the Cleveland-Akron
power grid caused the largest blackout in North American history, shutting
down electricity
from the Midwest to New York City. In the simplest terms, that is comparable
to the body’s reaction after spinal cord injury. Bones heal, but
damage to the power grid that is the central nervous system (CNS) has
devastating consequences.
The CNS, composed of the brain and the spinal cord, coordinates the body’s movement and sensation. The spinal cord is composed of neurons (also called nerve cells), which have three parts: a cell body; an axon, a long nerve fiber that grows out of the neuron; and dendrites, shorter processes that emerge from the cell body. The axon transmits and the dendrite receives communications from other cells.
Neurons communicate with each other by sending chemicals, called neurotransmitters, across a tiny space, called a synapse, between an axon and a dendrite. Neurons also travel by using chemical signals. Certain molecules on the surface of specific cells called adhesion molecules bind with similar molecules on nearby glial, or supporting cells, or axons. These chemical signals guide the axon to its final location. Axons also use chemical signals to help grow very long distances to their targets, for example, from the brain to the spinal cord.
 |
||
 |
||
After an injury, some of the astrocytes can form a “glial scar” that proves daunting to an axon. The glial scar serves “perhaps to block or wall off an injury site” after trauma, says Lemmon, but axons cannot grow on or move around these glial scars. “It’s like running into a wall—they (the axons) just can’t get through it.”
If everything is working correctly, the body’s internal circuitry keeps things moving along smoothly. “If you want to move your arm, you need a connection from your brain that says, ‘I want to move my arm,’ and then you need a connection to the spinal cord to move that limb. And then your arm moves,” says Bixby. But if the connection is damaged, the cells can’t communicate with one another and they can’t figure out what to do.
After a spinal cord injury (SCI), CNS neurons lose their connection to nerves located below the site of injury. These neurons may still be alive, but they’ve lost their ability to communicate and to control movement.
Once damaged, nerve cells in the central nervous system also lose their ability to regrow—or so it was thought until recently. In the last two decades, scientists have shown that nerve cells in the brain and spinal cord can regrow under certain conditions.
 Bixby and Lemmon are pursuing two lines of research
to develop novel treatments for spinal cord injury. They want to discover
how to influence nerve fibers
to regenerate across long distances and how to make meaningful connections.
Bixby and Lemmon are pursuing two lines of research
to develop novel treatments for spinal cord injury. They want to discover
how to influence nerve fibers
to regenerate across long distances and how to make meaningful connections.
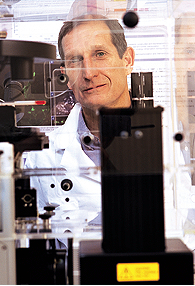
BIXBY AND LEMMON CONVERGE
![]()
few years ago, Bixby was working in the Department
of Molecular and Cellular Pharmacology at the School of Medicine, and
Lemmon was a professor of neuroscience
at Ohio’s Case Western Reserve University.
One of Bixby’s areas of research was exploring the ways in which specific neural connections are formed and maintained. Specifically, he looked at axon growth regulation and the control of synapse formation at neuromuscular junctions. Bixby was trying to find how the nerve cells make the appropriate connections—and how those synaptic wires are strung—so that when your brain tells you to move your arm, you move your arm and not your leg.
 Originally a “dyed-in-the-wool cell biologist” with an interest
in neural development, Bixby was drawn into this field because of its potential
in the treatment of spinal cord injuries. It was a new way of thinking
for the scientist. Through graduate and post-graduate work, Bixby conducted
basic science research without much interest in how his findings could
be used in medicine. But as he delved more into the neurosciences, he began
to see how therapies could evolve and he was “seduced by this idea
of clinical research.”
Originally a “dyed-in-the-wool cell biologist” with an interest
in neural development, Bixby was drawn into this field because of its potential
in the treatment of spinal cord injuries. It was a new way of thinking
for the scientist. Through graduate and post-graduate work, Bixby conducted
basic science research without much interest in how his findings could
be used in medicine. But as he delved more into the neurosciences, he began
to see how therapies could evolve and he was “seduced by this idea
of clinical research.”
“Scientists are largely driven by wanting to know the answers. We just want to know stuff,” Bixby says. “But we also want to know stuff that’s useful. If you can pursue your thirst for fundamental knowledge and at the same time have it be useful, that’s quite a combination.”
Meanwhile, Vance Lemmon was taking his own look into nerve cells. As a postdoctoral student at Washington University in St. Louis, Lemmon was more interested in cell biology and neural development than axons, but his interest in that area of neuroscience would be sparked by his colleagues in St. Louis. One of the top neuroscience researchers at Washington University was a gracious host who enjoyed fostering stimulating conversation among guests she invited to her home. That fellow scientist was Mary Bartlett Bunge, Ph.D.
Bunge would leave St. Louis to move to Florida and join the research team at the University of Miami, where she is now the Christine E. Lynn Distinguished Professor in Neuroscience as well as a professor in cell biology and anatomy and neurological surgery and neurology. She made a lasting impression on the young Lemmon.
In the late 1980s, Lemmon and his colleague Carl Lagenaur were working in the anatomy department at the University of Pittsburgh when they discovered that a certain adhesion molecule and receptor found in nerve cells (dubbed “L1”) stimulates axon growth. “L1 signals neurons to make them want to send out axons,” says Lemmon. “L1 is the switch that tells neurons to send specific signals that make axons grow as well as direct the axons to where they need to go.” This was the first adhesion molecule from the brain shown to have this property, pointing the way to several promising approaches for future research.
Last summer, Lemmon was named UM’s Walter G. Ross Chair in Developmental Neuroscience. In June 2003, Lemmon and Bixby joined The Miami Project to Cure Paralysis and teamed up to create the Laboratory for Axon Growth and Guidance, otherwise known as the Lemmon/Bixby Lab. Each scientist’s team works on individual projects stemming from the researchers’ previous work, such as honing in on the properties of L1, and on joint projects, where the two teams focus on how cell adhesion molecules can promote axon growth and influence axon guidance.
Bixby and Lemmon also were able to pool their financial resources to purchase sophisticated, state-of-the-art—and previously out of reach—laboratory equipment.
Two such instruments, the Cellomics KineticScan HCS Reader and the QIAGEN BioRobot 3000, are key tools for their studies and significantly reduce the time to conduct research. The QIAGEN BioRobot composes different concentrations of 6,000 drug compounds to determine if they have an effect on the cells. By hand, it would take countless hours to investigate these thousands of compounds. “You could not do four a day,” Lemmon says. The BioRobot could look at 1,000 per day.
The Cellomics Reader, relatively new technology which is available at only a handful of major research institutions, rapidly reads and analyzes pictures of cells to measure any axon or dendrite changes.
The two pieces of equipment together gather and analyze a huge amount of information for the researchers. Scientists realized early on that they had to investigate tens of thousands of drugs to find a “magic bullet,” but that kind of exhaustive research would require far more time and scientists than anyone was willing to commit.
“Ten years ago, I thought this was crazy. I thought it was too difficult to do,” says Lemmon. Not anymore. It is not possible to overestimate the impact new technology has had on spinal cord injury research. “It’s taken years off the process,” he adds. “Smaller and smaller groups of people can work on bigger projects.”
Still, given the complexity of SCI, researchers in the field have since concluded that there is no single magic bullet. “But I didn’t think ten years ago you could find the ten magic bullets that could push things through,” Lemmon says.
Technology, techniques, and closer ties between basic and clinical researchers are helping neuroscientists zero in on a cure for spinal cord injury. Bixby and Lemmon now see no limit to the research they can undertake. Says Bixby, “This is just the beginning.”
Robyn Nissim is an editor in the Office of Communications at the School of Medicine. Illustration by Nicholas Wilton. Photography by Mario Morgado.