
overcoming economic and cultural
barriers
Do-It-Yourself Cervical Specimens
 |
|
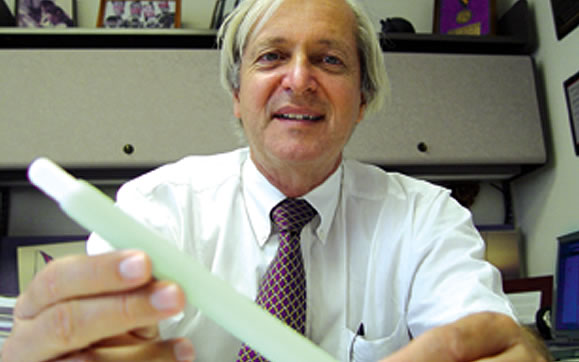
![]() he days of enduring the discomfort and embarrassment of a pelvic examination
for routine gynecologic screening may be numbered. A cervical self-sampling
device for detection of cancer and sexually transmitted infections, invented
by Arthur Fournier, M.D., vice chair in the Department of Family Medicine
and Community Health and associate dean for community health, is showing
positive results.
he days of enduring the discomfort and embarrassment of a pelvic examination
for routine gynecologic screening may be numbered. A cervical self-sampling
device for detection of cancer and sexually transmitted infections, invented
by Arthur Fournier, M.D., vice chair in the Department of Family Medicine
and Community Health and associate dean for community health, is showing
positive results.
A study published in The Journal of Reproductive Medicine found the Fournier Device could provide an efficient method of screening women in resource-poor countries or when cultural barriers exist to the use of traditional sampling methods, such as the Pap smear.
“In many resource-poor countries the access to routine cervical cancer screening is nonexistent, and even in some countries with well-established health care systems, patients choose not to be screened for cultural reasons,” explains Fournier. “This device is relatively inexpensive and can be used at home or at a doctor’s office. It may provide an efficient method of screening women not only in underdeveloped countries, but also in places where the traditional sampling methods run into cultural barriers. Ultimately the goal is to make this an option for all women.”
The Fournier Device is designed to be easily used by women themselves to obtain specimens. In the study, researchers compared the device with traditional sampling using cytologic and molecular-based tests for chlamydia, gonorrhea, and human papillomavirus (HPV), believed to be the cause of cervical cancer.
The study was performed in rural Haiti, among women who had never been screened before. The self-collected samples showed an overall increase in the number of cells collected and identified more cases of HPV than the traditional sampling method. Most importantly, the results of the two methods for detecting abnormal cells and the high-risk subtypes that cause cervical cancer were equivalent.
A second study focused narrowly on using the device as a test for HPV, and similar results were found. The National Cancer Institute is using the device in a demonstration project in rural Mississippi.
Major Advancement in Treating Sarcomas
The new facility has three main components: clinical services, a basic science laboratory, and the world-renowned UM Tissue Bank. “It’s a wonderful opportunity to have this kind of clinical and scientific enterprise all under one roof,” says H. Thomas Temple, M.D., chief of orthopaedic oncology and co-director of the UM Tissue Bank. “Particularly exciting is our basic science component. We will have some of the country’s top researchers working to understand the biology of tumors.” The Laboratory for Sarcoma Biology has a central scientific focus of better understanding tumor cell regulation and how it can be altered by the surrounding tissue. The laboratory will use state-of-the-art molecular and cellular biology techniques to evaluate cellular regulation and the process of tumor metastasis. The team’s three orthopaedic oncology surgeons and basic scientists have published hundreds of peer-reviewed articles in prestigious journals and been awarded millions of dollars in funding from the National Institutes |
Researchers Pose Ethical Questions about lethal injection
Cruel and Unusual Punishment?

![]() letter
written by researchers at the Miller School of Medicine and published in
The Lancet raises serious questions about lethal injection as a form of
capital punishment. The letter in the April 16 edition of the prestigious
international journal described compelling evidence of inadequate anesthesia
during executions.
letter
written by researchers at the Miller School of Medicine and published in
The Lancet raises serious questions about lethal injection as a form of
capital punishment. The letter in the April 16 edition of the prestigious
international journal described compelling evidence of inadequate anesthesia
during executions.
Lethal injection generally consists of the sequential administration of sodium thiopental for anesthesia, pancuronium bromide to induce paralysis, and finally potassium chloride to stop the heart and cause death. Without adequate anesthesia, the researchers conclude, the condemned person would experience suffocation and excruciating pain without being able to move or communicate.
“Unlike in medical applications, anesthesia in execution has not been subjected to clinical trials or government regulation, nor have the practitioners received even basic training to do this,” says David A. Lubarsky, M.D., M.B.A., professor and chairman of the Department of Anesthesiology and one of the letter’s authors. “This caused us to wonder whether anesthesia methodology in lethal injection might be inadequate.”
The research team—which also included UM faculty Teresa Zimmers, Ph.D., and Leonidas G. Koniaris, M.D., and Virginia attorney Jonathan Sheldon, who specializes in the legal defense of the condemned—used a combination of state records obtained under the Freedom of Information Act, along with personal interviews and sworn testimony of corrections officials involved in executions in Virginia and Texas. They also obtained autopsy toxicology results from 49 executions in Arizona, Georgia, North Carolina, and South Carolina.
Forty-three of 49 executed inmates had postmortem blood anesthesia levels below that required for surgery, while 21 of those inmates had levels that were consistent with awareness.
“The practice of lethal injection for execution perverts the tools of medicine and the trust the public has in drugs and clinical protocols,” says Koniaris, associate professor of clinical surgery, cell biology and anatomy, and lead author of the letter.
Honoring the Memory of Jay W. Weiss
![]() uring his lifetime Jay W. Weiss was a passionate and dedicated supporter
of the Miller School of Medicine and Jackson Memorial Hospital. He
died of cancer in January 2004, and this summer the Miller School
and Jackson honored his memory at a special tribute celebration.
uring his lifetime Jay W. Weiss was a passionate and dedicated supporter
of the Miller School of Medicine and Jackson Memorial Hospital. He
died of cancer in January 2004, and this summer the Miller School
and Jackson honored his memory at a special tribute celebration.
“Jay’s passing was an incalculable loss to this medical center, as well as the underserved and less fortunate in our community,” said John G. Clarkson, M.D., senior vice president for medical affairs and dean of the Miller School of Medicine, during the ceremony dedicating a sculpture of the longtime philanthropist and the naming of the Jay W. Weiss Ambulatory Care Center at Jackson.
“The dedication of Jay’s sculpture in the middle of the medical center is symbolic of the love and devotion he had for both institutions and those who work here,” the dean said.
Overall, Weiss helped raise more than $150 million for UM and Jackson, including millions in his own special contributions. He was a University trustee and a former chairman of the Miami-Dade County Public Health Trust, which oversees Jackson Memorial. In his business life, he built Southern Wine and Spirits into the country’s largest liquor distributor.
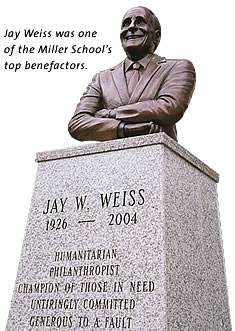 The sculpture is the work of artist Ric Frignoca
of Bronzeart in Sarasota. The renaming of the ambulatory care center
in Weiss’s name is a
constant reminder of his fundamental belief that no one should
be denied good medical care because of his or her socioeconomic circumstance.
The sculpture is the work of artist Ric Frignoca
of Bronzeart in Sarasota. The renaming of the ambulatory care center
in Weiss’s name is a
constant reminder of his fundamental belief that no one should
be denied good medical care because of his or her socioeconomic circumstance.
Weiss’s handpicked successor as advocate for the medical school, trusteeNorman Braman, said, “It is important to follow in Jay Weiss’s footsteps. [But] there was one Jay Weiss, and there will never be another.”
Seen and Heard across the nation
Making Headlines
Lethal Injection in The Lancet
 |
||
A letter written by researchers from the Miller School of Medicine and published in The Lancet raised serious questions about lethal injection as a form of capital punishment and garnered headlines around the world. The work done by Leonidas Koniaris, M.D., Teresa Zimmers, Ph.D., and David Lubarsky, M.D., suggested that inmates suffered during execution. The team was quoted extensively in every major national newspaper, including The Los Angeles Times, The New York Times, The Chicago Tribune, The Washington Post, The Seattle Times, and The Houston Chronicle. Reuters and the Associated Press also ran stories, as did ABC.com and MSNBC.com.
Internationally, the story got even more attention, with newspapers around the world picking it up. The Daily Telegraph, The Daily Mail, The Australian, and the BBC were just a few of the news outlets that did stories. RTL, a television network in Germany, traveled to Miami to interview the researchers, as did a news team from Antena 3 TV, Spain’s largest commercial television network.
Experts Comment on Terri Schiavo Case
Faculty from the Miller School of Medicine were front and center in newspapers and on television and radio programs in South Florida and across the country talking about the case of Terri Schiavo. The brain-damaged Florida woman, at the center of a seven-year end-of-life dispute among her family members, died March 31.
Kenneth Goodman, Ph.D., director of the University’s Bioethics Program, appeared on NBC Nightly News, ABC World News Tonight, The Diane Rehm Show on National Pubic Radio, and Voice of America, to name just a few. He was also quoted in every major newspaper in Florida, including The Miami Herald, the Sun-Sentinel, The Orlando Sentinel, and The Palm Beach Post, along with several national newspapers such as The New York Times and The Los Angeles Times.
 |
||
Walter Bradley, D.M., F.R.C.P., also was interviewed extensively about the definition of a vegetative state. Among the many interviews he did was for a full-page story in the Sun-Sentinel that included photos of court-obtained brain scans of Terri Schiavo used during the long legal battle.
Panagiota Caralis, M.D., appeared on MSNBC to talk about death and dying issues; John Kuluz, M.D., and Michael Nares, M.D., did numerous newspaper interviews to explain what happens when a feeding tube is removed; and Michael Norenberg, M.D., answered media questions about what could be expected from the Schiavo autopsy.
Faculty Garner National TV Exposure
Medical stories produced by WTVJ-TV medical reporter Diana Gonzalez about faculty members often get exposure across the country when they are sent via satellite to the NBC national newsfeed service. A story reported by Gonzalez on the Fournier Device invented for cervical cancer screening by Arthur Fournier, M.D., aired in 48 cities across the country, including Los Angeles, Chicago, and Boston.
A story by Gonzalez on the grand opening of the new orthopaedic oncology facility that featured H. Thomas Temple, M.D., aired in 20 cities across the country, including every television market in the state of Florida. The office staff reported a big increase in patient calls shortly after the stories aired.
Gonzalez produced a third story about laboratory
research on ubiquinone, commonly referred to as coenzyme Q10 or
CoQ10, as a possible cancer
fighter. The story on the research in the Department
of Dermatology and Cutaneous
Surgery aired in Miami and every other television market
in
Florida, in addition to 30 other cities, including
Houston, San Francisco,
Washington, D.C., and
Seattle.
 |
|||
 |
|||
JAY S. SKYLER, M.D., HONORED BY ACP
A Master Among Physicians
 |
||
![]() ay S. Skyler, M.D., first started working in diabetes
research as a third-year medical student. He was part of a team evaluating
an experimental surgical procedure to preserve eyesight in people with
type 1 diabetes.
ay S. Skyler, M.D., first started working in diabetes
research as a third-year medical student. He was part of a team evaluating
an experimental surgical procedure to preserve eyesight in people with
type 1 diabetes.
“I went around and met some of the patients with the diabetes team, and what struck me was that these people coming for this desperation procedure were my age, late-teens and 20s,” recalls Skyler. “That was pretty impactful.”
Skyler, professor of medicine, pediatrics, and psychology at the Miller School of Medicine, has since made an impact himself as a worldwide leader in diabetes research. Now he has joined the exclusive ranks of Master of the American College of Physicians (ACP).
Of approximately 116,000 total ACP members worldwide, only 564 are currently masters. According to ACP bylaws, masters are elected “on account of personal character, positions of honor, contributions toward furthering the purposes of the ACP, eminence in practice or in medical research, or other attainments in science or in the art of medicine.”
![]()
Skyler was in a class of 54 new masters honored at the annual meeting of the ACP in San Francisco. He became only the seventh faculty member in the history of the Miller School of Medicine to be selected.
Early in his career, Skyler and some colleagues devised a chart to help kids with diabetes record glucose levels, which let them adjust insulin injections. The chart became the Skyler Algorithms, now a core of diabetes education and management.
Now he directs the Type 1 Diabetes TrialNet, with 18 major research centers and many more community physicians, which is the latest achievement in a storied career that earned him this latest honor from the ACP.
“It’s a nice elite group, so I’m happy to join it,” he says.
Iron Arrow Lands on the Medical Campus On the Coral Gables campus, the tapping ceremony culminates at the Iron Arrow Mound. But until recently, few medical students were tapped for Iron Arrow. There was no ceremonial mound on the medical campus—and until ten years ago, no space to create one. “The medical school was considered out of sight, out of mind,” says Adam Blomberg, B.S. ’00, M.D. ’04. In 1993 Iron Arrow started tapping medical students, and 12 years later, after an intensive fundraising effort, the Miller School of Medicine finally unveiled an Iron Arrow site of its own. There are close to 200 Iron Arrow members on the medical campus—and with the new ceremonial circle on the campus, it’s likely many more will join that elite group.
|
Photos by Pyramid Photographics (Iron Arrow), Kelly Kaufhold (Fournier), John Zillioux, and by Veer,
 The
goal of the Miami Sarcoma Group is to effectively diagnose
and treat cancers of the bone and muscle. There are more than
600 different
possible diagnoses, and the locations can range from the spine
and pelvis to extremities including the hands and feet. The
group strives
to preserve or restore function after surgery, with limb salvage
possible in more than 85 percent of patients with malignant
diagnoses.
The
goal of the Miami Sarcoma Group is to effectively diagnose
and treat cancers of the bone and muscle. There are more than
600 different
possible diagnoses, and the locations can range from the spine
and pelvis to extremities including the hands and feet. The
group strives
to preserve or restore function after surgery, with limb salvage
possible in more than 85 percent of patients with malignant
diagnoses.