BY KERTING TRUJILLO BALDWIN
 HERE
WAS A TIME when an injury to the body, the brain, or the spinal
cord meant the end of an active life for many individuals. Medical
advances fell short and patients were left to cope with the loss
of a limb, the limitations of their muscles' strength, and the
inability to command their bodies to the smallest of tasks.
HERE
WAS A TIME when an injury to the body, the brain, or the spinal
cord meant the end of an active life for many individuals. Medical
advances fell short and patients were left to cope with the loss
of a limb, the limitations of their muscles' strength, and the
inability to command their bodies to the smallest of tasks.
Such times are history at the University of Miami School of Medicine, where orthopaedic surgeons, physicians, and physical therapists help patients every day to regain independence. From surgeries aimed at relieving spastic muscles to the retraining of nerve cells that survived spinal cord injury to the exercises aimed at helping amputees manage new prostheses, doctors are doing whatever it takes to reestablish function in patients who have the working parts but need a bit of tweaking, rewiring, or reengineering.
"When somebody has a devastating stroke, brain injury or spinal cord injury, or loses a leg or an arm, that's a tremendous blow to them-not just physically but mentally," says Mark Brown, M.D., chairman of the Department of Orthopaedics and Rehabilitation. "Nobody can cope with that alone, so the first thing we do is restore hope. And, you restore hope by getting patients to use the muscles that they have left and retrain them to their full potential."
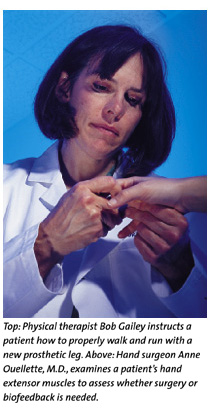
Gaining and maintaining enough function to perform everyday tasks such as bathing and eating is crucial and a goal in any rehabilitation. Spastic arm muscles are top culprits in limiting patients to perform daily activities. Hand surgeon Anne Ouellette, M.D., and psychologist Bernard S. Brucker, Ph.D., A.B.P.P., have handled hundreds of cases in which every spasticity is corrected either through surgery or biofeedback, a computer-assisted procedure that teaches the brain to use existing cells more efficiently to reestablish function.
"After an injury, you might have extensor muscles that are functioning, but the tension of the flexors is so tremendous that the muscle never relaxes," says Dr. Ouellette, chief of the hand surgery division at the School of Medicine. "Patients might be able to overcome their spasticity just by strengthening their extensor muscles, and if that is the case, we don't need to do surgery-just biofeedback."
Biofeedback works on the premise that some motor neuron cells or brain cells used for body movement actually survive after nervous system damage, and that these cells need retraining to help patients gain function. Biofeedback, also used in the rehabilitation of spinal cord injury patients, is essentially a "trial-and-error learning" technique-the same type of method people use subconsciously in learning to ride a bicycle, says Dr. Brucker, associate professor of clinical psychiatry at the School of Medicine. The computer, which is connected to the patient's body through a series of electrodes, charts the progress, displaying immediate and accurate feedback of the results after each attempt.
"Our work is to find the neural path to a muscle site and make a connection to produce action," Dr. Brucker says. "This work measures actual physiological responses to learning."
![]() f surgery
is the only answer, there are upper extremity procedures that
help patients gain mobility in the arms. Two of these procedures
are known as phenyl nerve block and flexor slide. The phenyl
nerve block uses a kind of alcohol solution that interrupts nerve
transmission for about six months. If a patient has better mobility
with the blocking of the arm nerves, hand surgeons cut the nerve
permanently, and the elbow is left to move freely.
f surgery
is the only answer, there are upper extremity procedures that
help patients gain mobility in the arms. Two of these procedures
are known as phenyl nerve block and flexor slide. The phenyl
nerve block uses a kind of alcohol solution that interrupts nerve
transmission for about six months. If a patient has better mobility
with the blocking of the arm nerves, hand surgeons cut the nerve
permanently, and the elbow is left to move freely.
 In
a flexor slide procedure, a muscle incision is made in the middle
of the humerus, which allows the forearm muscle to slide about
three inches toward the wrist, releasing tension and allowing
the wrist and fingers to extend. "It doesn't come out quite
normal, but good enough that a person can grab around a walker
or around the supports to get on or off a toilet," Dr. Ouellette
says. "All of a sudden that opens up a world of independent
care that they did not have."
In
a flexor slide procedure, a muscle incision is made in the middle
of the humerus, which allows the forearm muscle to slide about
three inches toward the wrist, releasing tension and allowing
the wrist and fingers to extend. "It doesn't come out quite
normal, but good enough that a person can grab around a walker
or around the supports to get on or off a toilet," Dr. Ouellette
says. "All of a sudden that opens up a world of independent
care that they did not have."
But in some cases, mobility is not the only factor at stake.
This is true for younger orthopaedic patients, such as 13-year-old
Jorge Figueroa. Until last year, Jorge was facing a future of
low back pain and other complications due to an uneven growth
in his legs. At age seven during an auto collision, he suffered
a growth plate injury of his right femur-the bone that connects
the hip and knee joints. By age 11, he needed a lift in his right
shoe to walk evenly because his right leg was two inches shorter
than his left leg.
Stephen Stricker, M.D., chief of pediatric orthopaedics at the School of Medicine, recommended the Ilizarov leg-lengthening technique for Jorge. Developed in Russia, the Ilizarov technique was first used in South Florida by Dr. Stricker in 1989. It utilizes a circular frame around the leg and has external knobs that lengthen the frame, thereby stretching the bone from each end.
"The bone is sliced somewhere in between points of attachment. The frame has 'clicker knobs' that the patient turns at home four times a day to gradually stretch the gap where the bone was cut," Dr. Stricker says. "The stretching is done so gradually that the body actually heals it by filling in the gap created as the bone lengthens."
"Jorge has already stretched his bone to the two inches he needed, and his bone formation is looking good," says his mother, Norma Torres. Young patients need to carry the circular frame for about eight months. Adult patients, however, must do so longer because their bones fill in the gap more slowly.
The Ilizarov technique has been a worthy method in restoring missing bone due to infection or trauma, eliminating the need for bone transplantation. It also has been used for lengthening short amputation stumps.
"For patients who have difficulty using a prosthesis because their forearm segment is too short to be able to flex the elbow, we can lengthen the forearm and make the prosthesis more usable for the patient," Dr. Stricker says.
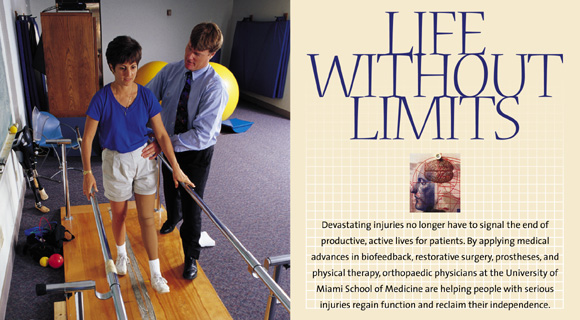
![]() nce the
prosthesis is in place, physical therapy becomes vital in teaching
patients how to manage their new body parts. School of Medicine
physical therapist Bob Gailey has been on the forefront of prosthetic
design and use, sharing his research and that of his colleagues
to encourage manufacturing companies to produce more functional
and better quality prostheses. Newer models now come with shock
absorption to dampen the impact of the ground, thanks to Gailey
and his physical therapy colleagues at the University. Gailey's
research also has bridged into the clinical areas, where he uses
training methods he developed to improve amputees' gait, reducing
the effort to walk.
nce the
prosthesis is in place, physical therapy becomes vital in teaching
patients how to manage their new body parts. School of Medicine
physical therapist Bob Gailey has been on the forefront of prosthetic
design and use, sharing his research and that of his colleagues
to encourage manufacturing companies to produce more functional
and better quality prostheses. Newer models now come with shock
absorption to dampen the impact of the ground, thanks to Gailey
and his physical therapy colleagues at the University. Gailey's
research also has bridged into the clinical areas, where he uses
training methods he developed to improve amputees' gait, reducing
the effort to walk.
"We restore their normal gait through exercises," Gailey says. "We help amputees integrate back into society without having them feel that people are looking at them differently."
The training first aims at restoring cardiovascular endurance and normal motion to the trunk and pelvis. Then, Gailey works on helping the patient gain balance, agility, and speed coordination. Finally, the patient goes through functional training in which he or she learns to master daily routines and is able to participate in recreational activities.
New medical developments are helping injured patients everyday
to return to mainstream society. With time, patients can lead
fuller lives through the help of these rehabilitative procedures.
"We are taking what patients have left after injury and
giving them back independence," Dr. Brown says. "It's
not a cure. The cure is in the test tubes. Meanwhile, we have
to rehabilitate. We have to try to teach them that the world
is not over and that life is not lost."
![]()
![]()
![]()
![]()
![]()