 hen Marc, a bright nine-year-old with asthma, is asked
why he's afraid to run laps in his gym class, his answer is somewhat
frightening. "Because I won't be able to breathe, and I'll
die," he says.
hen Marc, a bright nine-year-old with asthma, is asked
why he's afraid to run laps in his gym class, his answer is somewhat
frightening. "Because I won't be able to breathe, and I'll
die," he says.
Asthma is a problem. It's scary, and it's serious. Yet Marc is not alone. In fact, the legion of asthma sufferers grew from 6.7 million people in 1980 to 17.3 million in 1998, according to the Centers for Disease Control and Prevention (CDC). That's an alarming increase of 150 percent. Many of those numbers increased in the populations least able to fight the disease--underserved communities and their children. Approximately 40 percent of today's asthma population is under 18 years of age.
"If a parent needs to choose between food on the table and asthma medication, we face a losing battle," says Giovanni Piedimonte, M.D., F.C.C.P., associate professor in the Departments of Pediatrics, Medicine, and Pharmacology, and director of the Pediatric Pulmonary Division. "But we have powerful tools today, medications that if secured and used appropriately, work well. More than 95 percent of my patients, who understand the process and follow their treatment plan, are perfectly controlled."
So why aren't more children improving their asthma status? Because treatment, though largely successful today, only works if taken as directed. Many parents don't encourage their children to consistently take medications or perform the other preventive monitoring needed to keep asthma patients from having an attack, because they don't think it's necessary. This mindset is often counterproductive for patients and is one of the major hurdles to successful treatment.
"Unfortunately, asthma treatment requires adherence to complicated, lengthy regimens--taking several medications all serving different purposes, using peak airflow monitors and recording results, constantly carrying inhalers, using nebulizers to clear clogged airways. But the psychology of prevention is hard for many people to buy into," says Alan Delamater, Ph.D., director of the Division of Pediatric Psychology. "We can truly treat asthma today and may one day even prevent it, but all the strides in lab research can't make patients or parents comply. All this science can't make them appreciate being well."
Chronic illnesses, like asthma or diabetes, require patients to adhere to certain preventive measures now, to avoid suffering the consequences of the disease later.
"Getting kids and teens, and even parents, to understand that treatment is not only about getting rid of something, but preventing it from happening again, is a very hard concept," says Catherine Grus, Ph.D., a research assistant professor in the Department of Pediatrics and the pediatric psychologist in the Pulmonary Division.
Asthma is the leading cause of emergency room visits and hospitalizations for kids both nationally and at the University of Miami/Jackson Memorial Medical Center, and is the primary cause of school absences. Meanwhile, Marc is still afraid to run in gym class.
"Unfortunately, asthma has a tendency to create a population of couch potatoes and Nintendo players," says Dr. Piedimonte. "Fear of an asthma attack makes kids and parents avoid activities that can cause a problem, which drastically affects the whole family's quality of life. That's why we work with kids and parents to encourage the children to play in the band or participate in sports. We can adjust medications accordingly to keep them well."
In addition, continually avoiding therapy until a child arrives at the ER can cause permanent changes to the airways. Called remodeling, the condition occurs when patients delay the use of their preventive asthma medications (non-inflammatory steroids) over and over, allowing a serious attack to take place.
"The air passages (bronchi) eventually experience nonreversible structural changes that keep airways in a constant state of inflammation and can turn a moderate asthmatic into a serious case," says Piedimonte.
![]() istorically,
most asthma researchers studied the smooth muscle tissue in the
wall of the bronchial tubes, since constriction of this tissue
causes asthmatics to have difficulty breathing. Some 20 years
ago, University of Miami researchers were among the first to
target the lining of the airways, the epithelium, for study instead.
istorically,
most asthma researchers studied the smooth muscle tissue in the
wall of the bronchial tubes, since constriction of this tissue
causes asthmatics to have difficulty breathing. Some 20 years
ago, University of Miami researchers were among the first to
target the lining of the airways, the epithelium, for study instead.
"The epithelium is essentially the interface between the environment and the smooth muscle tissue," explains Adam Wanner, M.D., professor in the Department of Medicine and chief of the Division of Pulmonary and Critical Care Medicine, who has studied pulmonary disease and asthma at the School of Medicine for 25 years. "The smooth muscle is the target; that is what constricts to cause shortness of breath. But it is the epithelium that brings on that response from stimuli, or 'triggers,' like respiratory infections, cold weather, cigarette smoke, auto exhaust, dust, and others."
 University
of Miami researchers, in collaboration with William Abraham,
Ph.D., professor of medicine, Tahir Ahmed, M.D., professor of
medicine, and other faculty based at Mount Sinai Medical Center,
are using different strategies to understand how the airway epithelium
contributes to the clinical manifestations of asthma.
University
of Miami researchers, in collaboration with William Abraham,
Ph.D., professor of medicine, Tahir Ahmed, M.D., professor of
medicine, and other faculty based at Mount Sinai Medical Center,
are using different strategies to understand how the airway epithelium
contributes to the clinical manifestations of asthma.
Dr. Abraham has identified epithelium-damaging molecules, and Dr. Ahmed has discovered that heparin, a naturally occurring molecule in the body, has a protective effect in asthma. "Such findings are likely to lead to the development of new drugs for asthmatics," said Dr. Wanner.
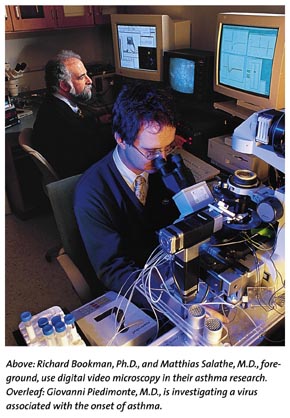
"We need to understand as much as possible about how the epithelium works to know what to target therapeutically," says Matthias Salathe, M.D., assistant professor in the Department of Pulmonary Medicine. "Steroids work well in treating asthma, but they provide a sledgehammer approach to therapy. If we can dissect this disease and target mechanisms that may not be working properly, we will one day have a better chance of having more directed treatment."
In a properly working respiratory epithelium, hair-like filaments on the surface of epithelial cells, called cilia, beat in a synchronized fashion to carry 150 milliliters of mucous out of our lungs on a daily basis. The average person swallows it throughout each day without even knowing. But, for asthma sufferers, secretions are produced faster than cilia can move them out. This increased amount of mucus in the airways makes the breathing tubes even narrower and overwhelms the regular system for cleaning out the airways.
Together with Richard Bookman, Ph.D., associate professor in the Department of Molecular and Cellular Pharmacology, Dr. Salathe has identified a method for measuring the beat frequency of cilia. Using digital video microscopy, their process measures light intensity changes as cilia move in and out of a designated viewing area. This system not only gives immediate feedback, but also is capable of tracing two cellular signals at the same time--the ciliary beat frequency, as well as a signal that controls beat frequency, for instance, the intracelluar calcium concentration. Only a few labs in the world are able to follow such signals at once.
"Since the 1970s, scientists have known how to measure beat frequency. We still know relatively little about how the cell regulates ciliary beat," says Dr. Salathe. "Our ability to watch two continuous activities is very significant since it helps to identify molecular targets of frequency regulation. One day we might be able to influence cilia to beat faster and stronger, in order to help move mucus out of the airways, even if the secretion makeup is suboptimal for transport."
![]() n the same
lab, University researchers are looking at two enzymes found
in mucous secretions. One, known as kallikrein, causes smooth
muscle to contract and constrict the airways. The second, called
lactoperoxidase, is an enzyme found in the airways that had not
previously been identified.
n the same
lab, University researchers are looking at two enzymes found
in mucous secretions. One, known as kallikrein, causes smooth
muscle to contract and constrict the airways. The second, called
lactoperoxidase, is an enzyme found in the airways that had not
previously been identified.
"This enzyme's major function is to prevent infections
in the airways," says Gregory Conner, Ph.D., associate professor
in the Department of Cell Biology and Anatomy, of work done collaboratively
with Rosanna Forteza, M.D., assistant professor in the Division
of Pulmonary Diseases. "This enzyme is also found in milk,
saliva, and tears."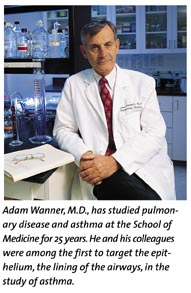
 Lactoperoxidase requires hydrogen
peroxide, which is produced by the airways. Interestingly, inflamed
airways produce even higher quantities, thereby increasing the
apparent activity of lactoperoxidase when it is most needed.
In fact, in animal models, medical school researchers have been
able to show that lactoperoxidase contributes significantly to
clear bacteria from the airways.
Lactoperoxidase requires hydrogen
peroxide, which is produced by the airways. Interestingly, inflamed
airways produce even higher quantities, thereby increasing the
apparent activity of lactoperoxidase when it is most needed.
In fact, in animal models, medical school researchers have been
able to show that lactoperoxidase contributes significantly to
clear bacteria from the airways.
"If we can keep bacteria from growing through the action of lactoperoxidase, we are giving cilia a chance and more time to clear the airways," says Conner, "especially if one day, through the work of Drs. Bookman and Salathe, we are able to influence beat frequency."
In other work, Dr. Piedimonte's lab is trying to elucidate the mechanism by which developing respiratory syncytial virus (RSV) infection within a child's first months, leads to persistent wheezing through age ten and beyond.
"Our interest in RSV derives from the fact that this is a virus encountered by half of the children on the planet in the first year of life," says Dr. Piedimonte, of the study published in the October 1999 issue of The American Journal of Physiology. His lab's work demonstrated that RSV increases the number of receptors binding an important mediator of airway inflammation. This mechanism may allow the virus to stay in a child's system for a short period of time, yet affect the airways for decades.
"In another study, to be published soon in Pediatric Research, we suggest that administering to high-risk infants an available antibody that works against RSV, called palivizumab, may protect against the airway inflammation associated with asthma," says Piedimonte. "If future clinical studies show what we've seen in animal models, we should be able to prevent many children from developing asthma."
Asthma research has advanced well in terms of treatment, but a shift is needed and emerging. "The American Thoracic Society (ATS) annually holds the world's largest meeting with regard to pulmonary medicine," says Dr. Wanner, ATS vice president.
"Twenty-five years ago, perhaps 25 percent of the presentations at ATS meetings were asthma-related. Today, the majority of papers deal with asthma. Our goal now is to make a paradigm shift toward prevention and cure."
and John Zillioux.