
Sharing Unique Insights from the World of Health Care Policy
Regional Academic Medical Center Established in Palm Beach County
Moving North
![]() irst
it was Bascom Palmer Eye Institute. Then UM/Sylvester at Deerfield
Beach.
irst
it was Bascom Palmer Eye Institute. Then UM/Sylvester at Deerfield
Beach.
 Now the expertise and excellence of all areas
of the University of Miami Miller School of Medicine will be reaching
beyond Miami-Dade County with
the signing of a historic agreement by Florida Atlantic University
(FAU), the Miller School, and Boca Raton Community Hospital.
Now the expertise and excellence of all areas
of the University of Miami Miller School of Medicine will be reaching
beyond Miami-Dade County with
the signing of a historic agreement by Florida Atlantic University
(FAU), the Miller School, and Boca Raton Community Hospital.
The agreement will create a regional academic medical center in Palm Beach County that should go a long way toward alleviating an expected physician shortage in Florida by expanding both undergraduate and graduate medical education, or residencies. Adding residency opportunities has proven to be the most effective way to increase the number of physicians in a region because doctors are likely to settle where they receive their graduate training. Local legislators have long asserted that the state doesn’t train enough young physicians to meet the needs in the state, particularly in Palm Beach County.
Currently, a group of University of Miami medical students attends the first two years of medical school on FAU’s Boca Raton campus before moving to the University’s medical campus for their final two years. The agreement calls for expanding the two-year program to a full four-year track in Boca, with clinical rotations at Boca Raton Community Hospital. The expanded program meets the state goal for more medical education opportunities without the expense of starting a new medical school.
Many of those physicians will be trained as part of the graduate medical education program to be established at Boca Raton Community Hospital, with an estimated 125 medical residents in the first year. To train the residents, the University of Miami Medical Group will establish a clinical faculty practice on the regional campus with at least 50 physicians.
“We promise all of you that the research, education, and training that our students will receive through this partnership will be second to none,” said UM President Donna E. Shalala. “The best kind of agreement brings together not only academic centers but the community, people who are familiar with the type of environment our young doctors may one day practice in.”
PI Program Finds New Home in Miami
Kleiner believes that the program will enable more outreach and help educate more physicians about PI. |
Podcasting delivers lectures online
Portable Learning
![]() n
2000 the Miller School of Medicine introduced video on demand and eliminated
the need for a “note service,” in which one student was
responsible for taking copious notes and distributing them to his or
her classmates. “We saved some trees,” says Nick Pikarsky,
director of the Biomedical Computing Office in the Department of Medical
Education.
n
2000 the Miller School of Medicine introduced video on demand and eliminated
the need for a “note service,” in which one student was
responsible for taking copious notes and distributing them to his or
her classmates. “We saved some trees,” says Nick Pikarsky,
director of the Biomedical Computing Office in the Department of Medical
Education.
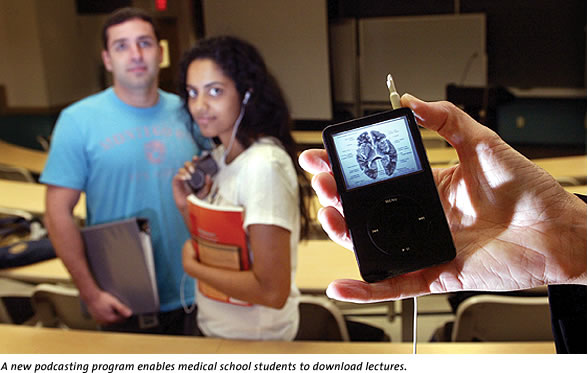
Video on demand enabled students to watch tapes of any of the 672 lectures held during the year whenever and wherever they needed.
Now the Department of Medical Education has gone a step further and is podcasting the lectures. A podcast is an audio file (MP3) that can be downloaded and listened to on a computer or portable player. Students subscribe to the medical school’s RSS feed (RSS, or Really Simple Syndication, is a standard way of tagging text and other content so that news readers and aggregators can siphon it from the Internet), and using free software, they can automatically download the latest audio files and import them into audio players. The introduction of the video iPod last November means that students will be able to view video podcasts when they’re on the go.
The podcasts, however, are not seen as a substitute for class attendance. “It’s no good if you don’t go to the lectures,” says second-year medical student Samantha Xavier. But the podcasts enable Xavier to study anywhere, anytime. And “it’s a lot easier to carry around than my laptop.”
Ron Clark, Ph.D., associate professor of cell biology and anatomy and coordinator for the neuroscience module, loves podcasting classes. He has even created mini-lectures for the iPods that work with audio alone or audio and video. “It’s the ideal study tool,” Clark says, noting that you can speed over the parts of a class you don’t need and repeat over and over the parts that you need. “I think students should learn any way that they can.”
You don’t need an iPod to listen to the lectures, though Pikarsky says at least 30 percent of the students do own the device. You would need software, such as iTunes or Windows Media Player for audio MP3 files or iTunes for video podcasts, and to subscribe to the RSS feed, you would need iTunes or Juice.
Freshman Pinning Ceremony Renamed for Clarkson
![]() ix
years ago, three students—Christine I. Pravia, M.D., Lakshmi
Reddy, M.D., and Jonathan Albert, M.D.—and then-president of the
University of Miami Medical Alumni Association, Steven Chavoustie, M.D.,
came up with the idea of establishing a pinning ceremony at the Miller
School of Medicine. The event, which officially welcomes the first-year
students to the study of medicine, was renamed this year in honor of
the Miller School’s dean emeritus, John G. Clarkson, M.D. Clarkson
was not only dean of the school during a ten-year tenure of unprecedented
growth—he is also an alumnus (M.D. ’68).
ix
years ago, three students—Christine I. Pravia, M.D., Lakshmi
Reddy, M.D., and Jonathan Albert, M.D.—and then-president of the
University of Miami Medical Alumni Association, Steven Chavoustie, M.D.,
came up with the idea of establishing a pinning ceremony at the Miller
School of Medicine. The event, which officially welcomes the first-year
students to the study of medicine, was renamed this year in honor of
the Miller School’s dean emeritus, John G. Clarkson, M.D. Clarkson
was not only dean of the school during a ten-year tenure of unprecedented
growth—he is also an alumnus (M.D. ’68).
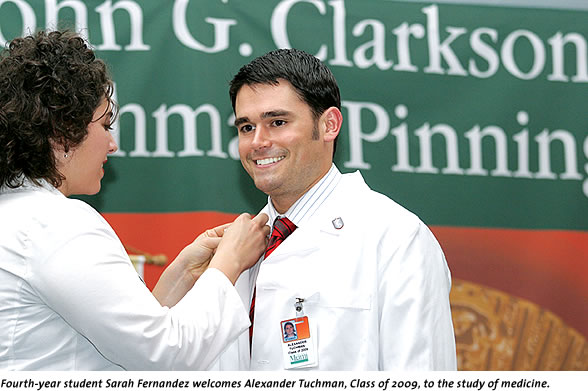
 “We celebrate this day at a truly remarkable
time in the history and development of the University of Miami Leonard
M. Miller School of Medicine,” Clarkson
said at the 2006 John G. Clarkson Freshman Pinning. “The expansion
begun just a few years ago is nearly ready to yield the first fruits
of our effort. Soon new buildings will change not only the campus landscape,
but the way we go about practicing the art and science of medicine. We
launch this acceleration at an opportune time in the history of medical
research and care. The pace of discovery is increasing exponentially,
offering the promise of new treatments and cures for our most intractable
diseases.”
“We celebrate this day at a truly remarkable
time in the history and development of the University of Miami Leonard
M. Miller School of Medicine,” Clarkson
said at the 2006 John G. Clarkson Freshman Pinning. “The expansion
begun just a few years ago is nearly ready to yield the first fruits
of our effort. Soon new buildings will change not only the campus landscape,
but the way we go about practicing the art and science of medicine. We
launch this acceleration at an opportune time in the history of medical
research and care. The pace of discovery is increasing exponentially,
offering the promise of new treatments and cures for our most intractable
diseases.”
Selected from a field of 3,740 applicants, this year’s 182-student freshman class is the largest in the school’s history. More than a third of the class were University of Miami undergrads.
Study Assesses Life after islet cell transplantn
Quality of Life Improves with Transplantation
![]() orty-year-old Rich Gurwitz of Kendall is forever grateful to have received
an islet cell transplant at the Diabetes Research Institute and to still
be off insulin more than four years later. “The feeling is hard
to describe,” Gurwitz says. “Nobody but a fellow diabetic
can really understand just what it means to undergo such a life-changing
procedure.”
orty-year-old Rich Gurwitz of Kendall is forever grateful to have received
an islet cell transplant at the Diabetes Research Institute and to still
be off insulin more than four years later. “The feeling is hard
to describe,” Gurwitz says. “Nobody but a fellow diabetic
can really understand just what it means to undergo such a life-changing
procedure.”
 Diagnosed at age 2 with type 1 diabetes, Gurwitz had
endured a lifetime of finger sticks and insulin injections, but the transplant
changed everything.
Miller School researchers have spent almost four years examining those
changes in Gurwitz and 22 other transplant patients.
Diagnosed at age 2 with type 1 diabetes, Gurwitz had
endured a lifetime of finger sticks and insulin injections, but the transplant
changed everything.
Miller School researchers have spent almost four years examining those
changes in Gurwitz and 22 other transplant patients.
Interviews and questionnaires were used to get a comprehensive gauge of the patients’ quality of life. They were evaluated while on the transplant waiting list and at selected intervals after transplantation.
Islet cell transplantation is considered the most promising method for curing diabetes. Islet cells are separated from a donor pancreas and infused into a patient’s liver, where they begin to produce insulin.
The study, authored by Rodolfo Alejandro, M.D., director of the clinical islet transplant program at the Diabetes Research Institute, and Raffaella Poggioli, M.D., assistant scientist, was published in the American Journal of Transplantation. It showed that despite all the patients had gone through, even if they had to go back on insulin they were still experiencing an improved quality of life three years later. All the patients reported less concern about their disease and said they were no longer living in fear of a sudden undetected and life-threatening drop in their sugar levels.
A Positive Paradox
But those studies focused on Mexican Americans in Texas and on the West Coast, not on the mix of nationalities in South Florida. His retrospective study of more than 80,000 births at Jackson Memorial Hospital found that Hispanics were the least likely to deliver prematurely and have low-birthweight babies compared with non-Hispanics (Asians), blacks, and white non-Hispanics. They were also more apt to seek care early in their pregnancies. This was the first study of its kind performed in South Florida and the largest by any single institution. The next step is to study factors such as acculturation, and socioeconomic, cultural, and genetic data to determine how and why this paradox occurs. “If we could figure out why this happens to Hispanics, we could apply it to other minorities,” says González-Quintero. “Our goal is to have an equal playing field for everyone in terms of pregnancy.” |
Program in Global Health Equity being launched
Opening Up a New World for New Residents
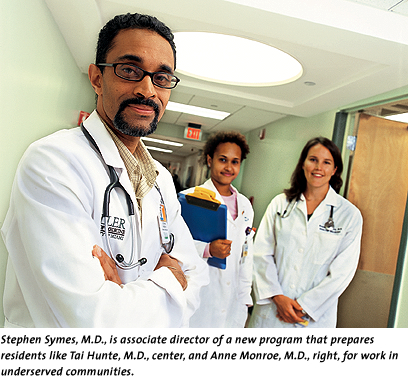
![]() n
addition to honing their skills as internal medicine physicians, two
young doctors will be receiving additional training in social medicine
this summer as the first residents in the Jay Weiss Residency Program
in Global Health Equity and Internal Medicine. The program is one of
several initiatives under way at the new Jay Weiss Center for Social
Medicine and Health Equity, which was established in honor of the late
philanthropist, a leading supporter of the Miller School of Medicine
and longtime champion of the less fortunate in our community.
n
addition to honing their skills as internal medicine physicians, two
young doctors will be receiving additional training in social medicine
this summer as the first residents in the Jay Weiss Residency Program
in Global Health Equity and Internal Medicine. The program is one of
several initiatives under way at the new Jay Weiss Center for Social
Medicine and Health Equity, which was established in honor of the late
philanthropist, a leading supporter of the Miller School of Medicine
and longtime champion of the less fortunate in our community.
Modeled after the Howard Hiatt Residency in Global Health Equity at Harvard University and Brigham and Women’s Hospital, the residency program aims to train physicians in the new field of health disparities, preparing them for work in underserved communities and with special populations. Paul Farmer, M.D., Ph.D., a Harvard medical anthropologist and physician as well as the founder of Partners in Health, heads the Howard Hiatt residency and will be providing input to the residency program as senior advisor to the Jay Weiss Center.
“Education was one of Jay Weiss’s most important priorities. He thought the best way to educate was by training others to be able to train others to be able to train others,” says Corinne Young, Ph.D., executive director of the Jay Weiss Center.
The training for the Jay Weiss residents will include fieldwork in sites serving the poor, research projects and mentorship, and immersion in the broad range of issues that affect global health. The residents will receive an M.S. in Public Health when they complete their residency.
The Jay Weiss Center is also introducing a new curriculum pathway in social medicine and health equity for medical students in the fall.
Sharing Unique Insights
from the World of Health Care Policy
![]() s
secretary of health and human services in the Clinton administration, Donna
E. Shalala was on the front lines when the nation began to focus on the
health care crisis.
s
secretary of health and human services in the Clinton administration, Donna
E. Shalala was on the front lines when the nation began to focus on the
health care crisis.

This past semester the University of Miami president shared her considerable experience with 250 students as she presented U.S. Health Care Crisis: Politics and Policy. The course was offered through the School of Nursing and Health Studies and was open to students from several different disciplines, including nursing, health science, premed, and political science. “There was a big demand for this course, and it filled up rather quickly,” says Anne O’Brien, B.S.N. ’04, a graduate student in the Family Nurse Practitioner Program who assisted President Shalala with the class. “The students know an information powerhouse when they see one.”
The course explored key health policy issues in the United States, along with the politics and interest groups that shape them. Major topics of discussion focused on Medicare, Medicaid, private insurance, the nursing shortage, and prescription drugs as well as the policies and politics surrounding bioethics, globalization, and infectious disease.
O’Brien says the course is an asset to anyone who is studying in a health-related field because it provides “context to the work they will be doing.”
 Seen
and Heard across the nation
Seen
and Heard across the nation
Making Headlines
Disclosing Biotech Problems
Robert J. Myerburg, M.D., professor of medicine, received coverage across the country for his role chairing the independent panel convened by Guidant Corporation to look into how they handled problems with their defibrillators. The Wall Street Journal and The New York Times had stories with Myerburg the day the report was released, and the Times followed up with a second story. Several television networks and at least 60 publications across the country picked up the story from wire services.
Lethal Injections Back in the News
Almost one year after researchers from the Miller School of Medicine raised serious questions about lethal injection and made headlines around the world, it was again back in the news. The study done by Leonidas Koniaris, M.D., Teresa Zimmers, Ph.D., and David Lubarsky, M.D., M.B.A., suggested that inmates suffer during execution, and it was recently cited in several high-profile court cases.
Lubarsky, chairman of anesthesiology, was interviewed extensively across the country about the developments. One television network, ABC, used him on three different programs. A Miami Herald profile of Lubarsky was picked up by 17 other newspapers across the country.
Detecting Bladder Cancer
A study co-authored by Mark Soloway, M.D., and published in the Journal of the American Medical Association showed that a simple test is highly effective to detect recurring bladder cancer. WFOR in Miami interviewed Soloway, and the story was aired by ten other TV stations across the nation.
 |
|||
 |
|||
Photos by Pyramid Photographics, Jenny Abreu (Modells), Kelly Kaufhold (Soloway), Biomedical Communicationsand Nuri Vallbona/The Miami Herald (podcasting) Additional photos by Donna Victor and John Zillioux (Gonzalez-Quintero).
 Patients
in Florida will now have a greater chance of receiving both the
diagnosis and treatment of PI with the opening of The Jeffrey
Modell Diagnostic Program for Primary Immunodeficiencies at the
UM
Miller School of Medicine. The program, one of only ten of its
type in the nation, is a collaboration between the Jeffrey Modell
Foundation
and Talecris Biotherapeutics.
Patients
in Florida will now have a greater chance of receiving both the
diagnosis and treatment of PI with the opening of The Jeffrey
Modell Diagnostic Program for Primary Immunodeficiencies at the
UM
Miller School of Medicine. The program, one of only ten of its
type in the nation, is a collaboration between the Jeffrey Modell
Foundation
and Talecris Biotherapeutics. Victor
Hugo González-Quintero, M.D., M.P.H., associate
professor of obstetrics and gynecology at the University
of Miami Miller School of Medicine, revisited the matter
in Miami. His
results, published in the Journal of Reproductive Medicine,
found that paradox to hold true, even with a different
Hispanic population.
Victor
Hugo González-Quintero, M.D., M.P.H., associate
professor of obstetrics and gynecology at the University
of Miami Miller School of Medicine, revisited the matter
in Miami. His
results, published in the Journal of Reproductive Medicine,
found that paradox to hold true, even with a different
Hispanic population.