 |
|
BY JOAN COCHRAN
|
|
“What exists here already, plus what we’re planning to add, can easily make this the best place in the world for Parkinson’s disease research,” says William C. Koller, M.D., Ph.D., professor of neurology, and national research director of the National Parkinson Foundation (NPF), who joined the UM team in 1999. Also recruited in 1999 was Abraham Lieberman, M.D., the national medical director of the National Parkinson Foundation and codirector of the UM/NPF Parkinson’s Disease Center. Author or coauthor of five books on Parkinson’s disease, he lectures widely on the subject and oversees the NPF’s national research and clinical programs.
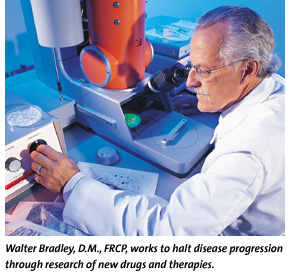
Drs. Koller and Lieberman currently are recruiting faculty and developing research projects to revitalize and expand the University’s Parkinson’s disease research and clinical efforts. As with most age-related neurological diseases, including Alzheimer’s disease and Lou Gehrig’s disease (amyotrophic lateral sclerosis), Parkinson’s disease occurs when nerve cells in the brain degenerate. In the case of Parkinson’s disease, cells that originate in the substantia nigra, at the base of the brain, degenerate and fail to release the neurotransmitter, dopamine. Scientists don’t know why these nerve cells die, but they do know that the symptoms of Parkinson’s disease—tremor, stiffness, slowness, shuffling, and loss of facial expression—stem from the dopamine deficiency. Unlike the other age-related degenerative diseases, Parkinson’s disease can be treated because the missing neurotransmitter can be replaced by Levodopa or L-dopa (Sinemet and generic analogs), a drug that is converted into dopamine in the brain. Dr. Lieberman and Walter Bradley, D.M., FRCP, professor and chairman of the Department of Neurology, were involved in early trials of this drug in the late 1960s. Dr. Bradley recalls the astonishment of those days. “Suddenly, women who’d been bed-bound for three to five years were getting up, cooking, losing weight, putting on makeup—it was a miracle of awakening,” he says, recalling the Robin Williams film Awakening, based on neurologist and author Oliver Sachs’ description of early use of L-dopa. “We thought L-dopa was the final cure for the disease. It would replace the lost dopamine and the disease would never return.” They were wrong. The cells of the substantia nigra continued degenerating, requiring that patients receive ever more frequent doses of L-dopa. By the end stage of Parkinson’s disease, many people began suffering from side effects of the drug. Instead of improving, many developed dyskinesia—writhing, wiggling movements that can make it impossible to bring a cup to your lips or stay balanced in a chair. End stage patients often experience a distressing “on-off” response in which they alternate, unpredictably and often within minutes, between the writhing movements of dyskinesia to complete immobility. “It’s pretty terrible and eventually can completely ruin the life of the patient,” Dr. Bradley says. “For the loved one, it’s a tremendous strain.” When Parkinson’s disease drugs no longer work, a relatively new technique called deep brain stimulation (DBS) can reduce symptoms, especially tremor, and improve a patient’s ability to function. While at the University of Kansas, Dr. Koller was one of the first in the United States to develop a surgical program utilizing DBS for Parkinson’s disease and tremor disorders. There, more than 200 tremor and Parkinson’s disease patients received DBS. Dr. Koller started a DBS program at the University of Miami, and, to date, more than 40 patients have undergone the procedure.
With a 1 percent to 2 percent chance of stroke, the procedure isn’t for everyone, Dr. Koller says. But in a dramatic video he shows patients, individuals with tremors that prevent them from holding a spoon or writing with a pen are capable of controlled activities once the electrodes are turned on. “I never knew when I’d be on or off, because the changes came so quickly. My arms would suddenly swing around, and I’d be afraid of hitting someone in the face,” Howard Watkins, a retired Internal Revenue Service executive, says of his swings from normal functioning to violent dyskinesia before undergoing the DBS procedure. “Now my dyskinesia is almost gone.” Dr. Koller and his colleague, Kelly Lyons, Ph.D., research assistant professor of neurology, are involved in the study of approximately 15 investigational drug therapies. This research includes the study of controlled release formulations of currently prescribed drugs, which would limit the number of drug doses per day; glutamine-blocking drugs, which could possibly reduce symptoms and slow disease progression; and an examination of the most appropriate time during the course of the disease to initiate various therapies to reduce drug side effects. They also are examining the genetic contributions to Parkinson’s disease. Dr. Koller is particularly excited about the University’s involvement in a six-month, 20-center trial of Amgen 474. When this nerve growth factor was given to animals, dopamine-producing cells that were dying returned to normal. By the end of the year, participants will know if the dopamine-producing cells also are rejuvenated in humans.
“Of all the biological frontiers, the brain has been the last, because you can’t obtain tissue from a living brain and there’s no animal model whose brain mirrors the human brain,” she says. The “million-dollar question” in Parkinson’s disease, according to Dr. Mash, is why neurons die off. “Is there a genetic signal that triggers the death of the neuron, or does the injury occur at a distal site of the brain?” she asks. “Are environmental causes, such as pesticides or head trauma, a factor?” Prospective brain donors are screened to single out genetic and environmental causes of diseases. Diseased tissue also is compared to that of “control” or normal brain tissue, which helps researchers identify differences in brain cells attributable to normal rather than premature aging. Dr. Mash is particularly concerned about the Parkinson-like symptoms seen in cocaine users, and predicts a wave of Parkinson’s disease as these users age. She also is doing very promising work on determining which genes influence the deposition of proteins within dopamine-forming cells, considered to be a factor in the death of these cells. Perhaps the most fascinating aspect of Parkinson’s disease research—apart from the promise it holds for better treatment and cures—is what it reveals about the aging process. “A whole litany of problems are caused by the age-related degeneration of nerve cells, from hearing and balance problems to retinal degeneration, Alzheimer’s disease, and Parkinson’s disease,” Dr. Bradley notes. “It’s very likely that when we get a complete understanding of what happens to damage the nerve cells in one disease, we’ll have a better understanding of all the others and of the aging process itself.” |
|
|
| Joan Cochran is a frequent contributor to the University’s alumni magazines. Photography by John Zillioux. |
|
|
|
|
|
|
|
|

 Nizam
Razack, M.D., a neurosurgeon, was jointly recruited by the Parkinson
center and the Department of Surgery to perform the DBS procedure. Dr.
Razack inserts electrodes through a tiny hole in the skull into the
patient’s globus pallidus or subthalamic nucleus, both of which
control movement, then wires them to a pulse generator implanted in
the chest wall. A handheld magnet is used to turn the system on and
off, and the system parameters can be adjusted during an office visit
to allow for better control of Parkinson’s disease symptoms as
necessary.
Nizam
Razack, M.D., a neurosurgeon, was jointly recruited by the Parkinson
center and the Department of Surgery to perform the DBS procedure. Dr.
Razack inserts electrodes through a tiny hole in the skull into the
patient’s globus pallidus or subthalamic nucleus, both of which
control movement, then wires them to a pulse generator implanted in
the chest wall. A handheld magnet is used to turn the system on and
off, and the system parameters can be adjusted during an office visit
to allow for better control of Parkinson’s disease symptoms as
necessary.