![]() ike
researchers in virtually every medical field, Craig Buchman, M.D., is
preparing for his world to be turned upside down. Dr. Buchman, an assistant
professor of otolaryngology, studies the causes of chronic middle ear
infections in children. Up to now it’s been slow going. But with
the release last June of preliminary findings in the ten-year, $3 billion
Human Genome Project, Dr. Buchman can now begin searching for a long-suspected
genetic link to the condition. Establishing that link, he explains, is
the first step toward developing gene-based therapies that could render
current treatments obsolete.
ike
researchers in virtually every medical field, Craig Buchman, M.D., is
preparing for his world to be turned upside down. Dr. Buchman, an assistant
professor of otolaryngology, studies the causes of chronic middle ear
infections in children. Up to now it’s been slow going. But with
the release last June of preliminary findings in the ten-year, $3 billion
Human Genome Project, Dr. Buchman can now begin searching for a long-suspected
genetic link to the condition. Establishing that link, he explains, is
the first step toward developing gene-based therapies that could render
current treatments obsolete.
“Having a template of the genetic makeup of humans, we can now begin looking at disease, and the causes of disease, in an entirely new way,” says Dr. Buchman. “It will be a world of medicine that was unimaginable only a few years ago.”
 Such
is the monumental promise of the Human Genome Project. Launched in 1990,
the project is an international effort by a team of biologists, biochemists,
computer scientists, and other experts to spell out the precise chemical
sequence constituting the DNA in every cell in the human body. Call it
an instruction manual for human life—a how-to guide listing the 80,000
or so genes that define our inheritable and physical traits. When complete,
it will help medical researchers attack the genetic roots of disease.
In time, new diagnostic procedures will pinpoint not just the cause but
the location of human illness. Treatments will be individually tailored
to each patient. Preventative medicine will begin at the time of, or even
before, birth. Other implications abound. The mapping of the human genome—widely
heralded as one of the greatest scientific achievements in history—will
change forever our relationship to the natural world by removing a biological
shroud from the components of human life.
Such
is the monumental promise of the Human Genome Project. Launched in 1990,
the project is an international effort by a team of biologists, biochemists,
computer scientists, and other experts to spell out the precise chemical
sequence constituting the DNA in every cell in the human body. Call it
an instruction manual for human life—a how-to guide listing the 80,000
or so genes that define our inheritable and physical traits. When complete,
it will help medical researchers attack the genetic roots of disease.
In time, new diagnostic procedures will pinpoint not just the cause but
the location of human illness. Treatments will be individually tailored
to each patient. Preventative medicine will begin at the time of, or even
before, birth. Other implications abound. The mapping of the human genome—widely
heralded as one of the greatest scientific achievements in history—will
change forever our relationship to the natural world by removing a biological
shroud from the components of human life.
In its present form, the so-called “road map of life” is not much to look at: page after page after page of the letters A, C, G, and T (some 3.2 billion characters in all) appearing in mysterious, code-like order. (The data released last June is essentially a rough draft. A final version should be completed by 2003). The letters stand for the four chemical bases that make up DNA—adenine, cytosine, guanine, and thymine. Buried within this vast string of letters, like a few sequential notes within a grand symphony, are each of the tens of thousands of genes that determine everything from our hair color to skin complexion to our susceptibility to cancer and other illnesses. To date, only a small fraction of all genes have been discovered. But now, scientists can begin scouring the code in search of others. This, in turn, could shed light on the causes and treatments of virtually any disease.
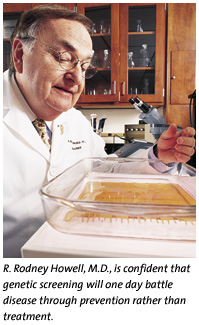
![]() he
implications for health care are tremendous,” says R. Rodney Howell,
M.D., chairman of the Department of Pediatrics at the School of Medicine
and president of the American College of Medical Genetics. “It will
take time to gather the full benefit of the Human Genome Project, but
this will no doubt change the practice of medicine in every way.”
he
implications for health care are tremendous,” says R. Rodney Howell,
M.D., chairman of the Department of Pediatrics at the School of Medicine
and president of the American College of Medical Genetics. “It will
take time to gather the full benefit of the Human Genome Project, but
this will no doubt change the practice of medicine in every way.”
For example, Dr. Howell, who also is interim director of the new Dr. John T. Macdonald Foundation Center for Medical Genetics at the School of Medicine, envisions a day when health care practitioners diagnose their patients by comparing a genetic sample to a control sample pulled from a catalog of all human genes. Differences will denote a specific disease. In limited cases this is already occurring. Using sophisticated genetic tests, researchers recently found that patients diagnosed with B-cell lymphoma respond differently to standard treatments because the disease, at the molecular level, can be vastly different. In essence, the research showed, what was once thought to be one disease is actually many. The findings have led to a search for new treatments.
Our knowledge of the genome also may help explain why some ethnic groups have a higher risk for certain diseases. Associate research professor Lisa Baumbach-Reardon, Ph.D., a genetic specialist at the School of Medicine, hopes to understand why there is a difference in gene mutation frequencies associated with breast cancer genes between African-American and Caucasian women. Two genes that play a role in hereditary breast cancer already have been discovered. Based on her research findings, Dr. Baumbach-Reardon believes others could exist. Researchers suspect that even common conditions like hypertension or a simple headache might have myriad genetic dispositions, each requiring different treatment.
 While
such research is both complex and costly, that’s expected to change.
One of the new genomics technologies makes use of an assay known as a
DNA micro-array. A single test in a private lab can take two days and
can cost upwards of $5,000. The University of Miami, like most major research
institutions, has its own facility to carry out these measurements. But
Richard Bookman, Ph.D., associate dean of the School of Medicine and director
of its DNA micro-array facility, says the cost of testing, and the hardware
itself, will come down as demand soars. Dr. Bookman envisions some of
this technology appearing in every doctor’s office. “The genome
isn’t just for geneticists anymore,” he says.
While
such research is both complex and costly, that’s expected to change.
One of the new genomics technologies makes use of an assay known as a
DNA micro-array. A single test in a private lab can take two days and
can cost upwards of $5,000. The University of Miami, like most major research
institutions, has its own facility to carry out these measurements. But
Richard Bookman, Ph.D., associate dean of the School of Medicine and director
of its DNA micro-array facility, says the cost of testing, and the hardware
itself, will come down as demand soars. Dr. Bookman envisions some of
this technology appearing in every doctor’s office. “The genome
isn’t just for geneticists anymore,” he says.
This and other predictions have spawned the term “individualized medicine” or “personalized medicine.” Not only will diagnosis be made with molecular accuracy, so will drug selection and dosage. Genetic screenings can help patients avoid adverse drug reactions by alerting the physician in advance of treatment. Dosages can be tailored precisely to each patient’s requirements.
These advances have given rise to the new field of pharmacogenomics. Drug makers expect a larger benefit: a reduction in drug-use complications may help win FDA approval of innumerable new drugs. Dr. Bookman explains: “If an experimental drug poses a risk to even a small percentage of people, it isn’t approved. But if we can determine which patients are not at risk, why not make the drug available to them?”
Advanced genetic screening also will promote preventative medicine. With a simple test, parents will know their infant’s inherited risks: What are the child’s chances of developing heart disease, Alzheimer’s, leukemia, or prostate cancer? This early awareness will translate into billions of dollars per year in reduced medical costs. “Medicine in the coming century will be all about prevention,” says Dr. Howell.
![]() ut
the fear of knowing one’s risks will likely be tempered by the vast
promise of gene therapy techniques. While early attempts have proved disappointing,
our ability to study the genome en masse—rather than one gene at
a time—is expected to open the doors to genetic engineering. Rather
than treat the symptoms of disease, why not insert, replace, alter, or
manipulate the genes causing the abnormality? Most scientists agree that
such therapies will be commonplace with the advance of yet another new
field, so-called proteomics—the macro-level analysis of the proteins
within the cell. Mapping the genome is the first step toward producing
a complete inventory of human proteins and their uses.
ut
the fear of knowing one’s risks will likely be tempered by the vast
promise of gene therapy techniques. While early attempts have proved disappointing,
our ability to study the genome en masse—rather than one gene at
a time—is expected to open the doors to genetic engineering. Rather
than treat the symptoms of disease, why not insert, replace, alter, or
manipulate the genes causing the abnormality? Most scientists agree that
such therapies will be commonplace with the advance of yet another new
field, so-called proteomics—the macro-level analysis of the proteins
within the cell. Mapping the genome is the first step toward producing
a complete inventory of human proteins and their uses.
 Proteins
are the chemical compounds of amino acids, which regulate much of the
body’s functioning. It can be an enzyme that helps digest food, a
neurotransmitter that allows brain cells to communicate, or an antibody
that helps fight infection. The primary task of most genes is the production
of these proteins. Kelvin Lee, M.D., associate professor of medicine and
microbiology and immunology at the School of Medicine, says the future
of proteomics is immense. Dr. Lee is exploring the idea that the body
can be cued to vaccinate itself against cancer. Proteins hold the key.
Proteins
are the chemical compounds of amino acids, which regulate much of the
body’s functioning. It can be an enzyme that helps digest food, a
neurotransmitter that allows brain cells to communicate, or an antibody
that helps fight infection. The primary task of most genes is the production
of these proteins. Kelvin Lee, M.D., associate professor of medicine and
microbiology and immunology at the School of Medicine, says the future
of proteomics is immense. Dr. Lee is exploring the idea that the body
can be cued to vaccinate itself against cancer. Proteins hold the key.
“If we can translate the human genome into the entire constellation of human proteins,” Dr. Lee explains, “then perhaps we can identify something that can attack tumors.”
While such discoveries will no doubt revolutionize medicine, our mastery of the human genome also raises ethical concerns. No one objects to new therapies, but how far should science go in revealing our genetic predispositions? Certainly all of us possess genes associated with adverse health conditions. Will our awareness of them create a kind of anticipatory hypochondria—a fevered rush to receive every possible genetic cure long before the malady arrives? Will fetuses be screened not only for Down’s syndrome and other serious genetic disease but also for bad skin and oily hair? The possibilities are endless.
We also may learn that many behavioral characteristics have genetic links. Would we want to screen prenatally for antisocial behavior or learning difficulties? Within a decade, researchers believe that a few drops of a pregnant woman’s blood—as an alternative to amniocentesis—will reveal a treasure trove of information about her fetus’ physiological and psychological makeup. That prospect, along with expected advances of in vitro fertilization, may give prospective parents the opportunity to select out all but strong, attractive, good natured, Ivy League-bound offspring. So worrisome are these and other concerns that a chunk of the Human Genome Project’s budget is earmarked for studies in bioethics.
“Many of us are very uncomfortable with the idea that we will use this newfound knowledge for enhancement purposes,” says Kenneth Goodman, Ph.D., director of the School of Medicine’s bioethics program. “But this is the kind of challenge that the great discoveries throughout history have posed. Science, in a sense, is rudderless. Now we have to set a course for ourselves.”
Illustration by Terry Miura. Photography by John Zillioux.