 |
|
|
BY HOLLY STRAWBRIDGE
|
|
|
A call made en route to the Emergency Department ensures that a University of Miami neurology resident is waiting. While the resident performs a quick assessment to rule out other medical conditions that produce stroke-like sym ptoms, the patient’s blood is drawn and an EKG is taken. Confirming the likelihood that a stroke has occurred, the resident pages a neurologist on the UM/Jackson Brain Attack Team. Meanwhile, the patient is rushed into radiology, where she is given priority over other patients for a CT scan of her brain. The neurologist is paged. He drops everything and runs to the Emergency Department. Immediately, he meets with the neuroradiologist to examine the patient’s CT scan. A clot has blocked a small blood vessel in her brain. Well under three hours have passed since this occurred, making the patient an ideal candidate for treatment with a clot-busting drug. The neurologist understands that the patient might benefit from one of many clinical trials of new drugs they hope will reduce the long-term damage from stroke. The Brain Attack Team’s nurse practitioner, Kathy Hesse, explains what the physicians will try to accomplish and requests the husband’s consent to proceed. He readily agrees. A few minutes later, lifesaving drugs are dripping into the patient’s bloodstream. Her strength gradually returns, and she becomes more alert. Thirty minutes later, she is speaking again. The crisis is over, and she is taken to Jackson’s Stroke Unit to be monitored overnight. Another life has been saved—and quality of life preserved—thanks to a stroke team that acted fast.
“Within the past five years, new treatments have developed that must be done within three hours. One example is the intravenous clot-busting drug tPA, now considered standard treatment. So we must be prepared to quickly make a diagnosis, exclude other possibilities, do a CT scan, assess if the stroke should receive treatment, institute that treatment, monitor for complications, and be able to deal with those that occur,” Dr. Forteza explains. “Our protocol enables us to act fast.” Strokes occur when brain cells are deprived of blood. Nearly 80 percent of strokes are caused by a blood clot that blocks an artery in the brain. Such clots tend to form in arteries that have become narrowed by atherosclerosis, the same process responsible for many heart attacks. In some patients, certain conditions can cause clots to form inside the heart’s chambers. These clots can break free and travel in the bloodstream to the brain, where they may also get stuck in a blood vessel. A small percentage of strokes occur when a vessel in the brain bursts, spilling blood into the brain tissue. This type of stroke often requires surgery to stop the bleeding or to remove clots that press on delicate brain tissue.
After patients have been admitted to Jackson, superb care is provided in the neurosurgical intensive care unit. Specially trained nurses staff the four-bed Stroke Unit. Physical, occupational, and speech therapists familiar with problems caused by stroke assess patients and start rehabilitation as quickly as possible. Social workers and home health coordinators help patients and their families prepare for life after the hospital. “We are without a doubt the best-prepared stroke center in town, probably in Florida,” says Dr. Forteza. For Dr. Forteza, the establishment of a pacesetting stroke center at UM/ Jackson was just the beginning of a crusade to make the highest-quality emergency stroke care available throughout the county. Energized by these dreams, the UM/Jackson stroke team invited Metro-Dade Emergency Medical Services (EMS), along with neurologists, neurosurgeons, emergency physicians, internists, radiologists, primary care physicians, nurses, physical therapists, and administrators from every local hospital, to join them in forming the Miami-Dade Stroke Coalition. The group is dedicated to improving the detection, treatment, and prevention of stroke throughout the county. The American Heart Association quickly joined the effort, bringing invaluable advice gleaned from other coalitions throughout the nation. Improvements in the existing system began immediately. The first order of business was to identify which hospitals could provide adequate emergency stroke care within six hours (designated Level I) and which could not (Level II). The law was then changed to allow EMS to take suspected stroke patients to a Level I hospital rather than the closest facility. “Who wants to go to a place where they are unprepared?” Dr. Forteza questions. “It doesn’t happen with heart attack or maternity patients. Why should it happen with stroke patients?” Level II hospitals hoping to become Level I simply need to make their desires known, and the UM/Jackson Brain Attack Team will provide the necessary guidelines, supervise their implementation, and train their personnel for free. This enormous effort is made in the same spirit in which the coalition was conceived: “Because it’s the right thing to do,” says Dr. Forteza. The American Heart Association agrees. They have seen the effectiveness of such coalitions nationwide, and joined with the Miami-Dade team to provide invaluable perspective from a national level. Stroke statistics are frightening. Stroke is the third leading cause of death and number one cause of disability, yet knowledge about stroke symptoms and treatment is poor. A questionnaire performed by the American Stroke Association in Miami-Dade County reported that among 262 individuals surveyed, only 15 percent recognized weakness and 13 percent recognized difficulty speaking as signs of stroke. For this reason, the coalition is planning to place information about stroke before the general public in every way possible and in many languages. In the near future, the Stroke Coalition hopes to prove that these monumental efforts are paying off. “For conditions like stroke, we must behave as a community and work together instead of against each other. When patients are seen and treated within three hours, word gets out and the public learns to call 911 right away,” says Dr. Forteza. “By acting fast, we can save many lives.” |
|
|
|
|
| Holly Strawbridge is a medical writer based in Fort Lauderdale, Florida. Photography by John Zillioux. | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
 red ambulance careens through Miami’s dark streets, its siren screaming
like a broken heart. On the stretcher lies a frightened 53-year-old
schoolteacher, whose husband found her weak, confused, and unable to
speak. The EMS technicians suspect she has had a stroke and have elected
to take her to Jackson Memorial Hospital. It’s nearly midnight
on a holiday weekend, but they know that Jackson, a Level I stroke center,
is always prepared.
red ambulance careens through Miami’s dark streets, its siren screaming
like a broken heart. On the stretcher lies a frightened 53-year-old
schoolteacher, whose husband found her weak, confused, and unable to
speak. The EMS technicians suspect she has had a stroke and have elected
to take her to Jackson Memorial Hospital. It’s nearly midnight
on a holiday weekend, but they know that Jackson, a Level I stroke center,
is always prepared.  In
the majority of strokes, however, acting fast to dissolve clots helps
restore blood flow. How quickly this happens determines the amount of
permanent damage a patient will suffer, since brain tissue deprived
of blood dies gradually from the center of impact outwards. Although
powerful clot-busting drugs work wonders when given within three hours,
they actually can do more harm than good when used inappropriately or
after this window of opportunity has passed. That’s why the ability
to quickly assess the type of stroke and timing of onset are critical.
By 1999 the Brain Attack Team included four fellowship-trained, University
of Miami cerebrovascular specialists—Jose Romano, M.D., Mauricio
Concha, M.D., Sebastian Koch, M.D., and Dr. Forteza—and nurse practitioner
Kathy Hesse, ARNP. Today, they screen an average of seven emergency
patients a day, in addition to hundreds of outpatients a year.
In
the majority of strokes, however, acting fast to dissolve clots helps
restore blood flow. How quickly this happens determines the amount of
permanent damage a patient will suffer, since brain tissue deprived
of blood dies gradually from the center of impact outwards. Although
powerful clot-busting drugs work wonders when given within three hours,
they actually can do more harm than good when used inappropriately or
after this window of opportunity has passed. That’s why the ability
to quickly assess the type of stroke and timing of onset are critical.
By 1999 the Brain Attack Team included four fellowship-trained, University
of Miami cerebrovascular specialists—Jose Romano, M.D., Mauricio
Concha, M.D., Sebastian Koch, M.D., and Dr. Forteza—and nurse practitioner
Kathy Hesse, ARNP. Today, they screen an average of seven emergency
patients a day, in addition to hundreds of outpatients a year. 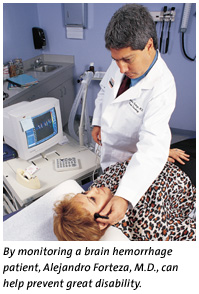 Sophisticated
ultrasound equipment enables them to help evaluate a patient’s
blood vessels and pinpoint the source of a stroke. “We are now
able to do a variety of noninvasive tests that assist in making revascularization
decisions and help identify patients at high risk for stroke,”
says Dr. Romano. “One of the machines is located at Jackson, where
we monitor individuals with brain hemorrhages to detect a condition
called preclinical vasospasm. This all-too-common condition leads to
great disability. Fortunately, it is treatable if detected early, which
we can do.”
Sophisticated
ultrasound equipment enables them to help evaluate a patient’s
blood vessels and pinpoint the source of a stroke. “We are now
able to do a variety of noninvasive tests that assist in making revascularization
decisions and help identify patients at high risk for stroke,”
says Dr. Romano. “One of the machines is located at Jackson, where
we monitor individuals with brain hemorrhages to detect a condition
called preclinical vasospasm. This all-too-common condition leads to
great disability. Fortunately, it is treatable if detected early, which
we can do.”