 |
|
 |
The
case of Terri Schiavo, a young Florida resident, would soon come to embody
both. It would also become the case that catapulted UM’s Ethics
Programs into the international spotlight.
Theresa Marie Schiavo slipped into a coma in 1990 in St. Petersburg, Florida. By 1993 her parents and her husband had a falling out over her care, and in 1998 her husband Michael Schiavo petitioned the court—for the first time—to have her removed from life-sustaining care because she was in a persistent vegetative state. Terri never wanted to live like this, he insisted. Her parents disagreed.
Several court orders and lawsuits later, Terri Schiavo became the unwitting symbol of both the right-to-die and the right-to-live movements.
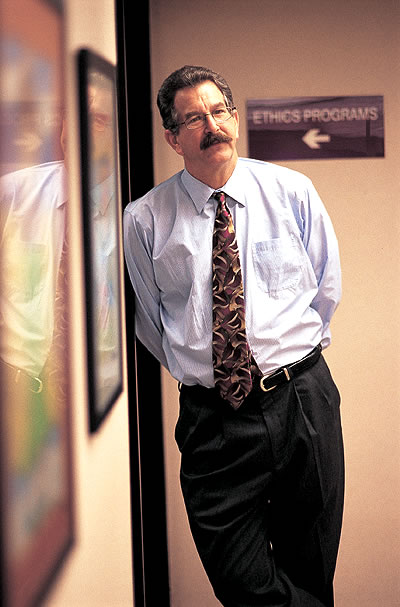
As her health deteriorated, Goodman was receiving his doctoral degree in philosophy from the University of Miami and working as adjunct faculty in the University of Pittsburgh Center for Medical Ethics, one of the few established programs in the country. He was inspired and came back to UM with a mission.
“We need to start an ethics program at the School of Medicine and I hope to build it into one of the finest in the country,” he told school officials. Goodman’s desire to create such a program was considered by many to be ambitious—and by others to be completely unrealistic.
The school’s administrators went with ambitious. In 1992 Goodman was given a desk, a phone, and a computer and was told to build a program. It turned out to be a prescient decision.
“The goal was to create an entity that could be listed among the other great ethics programs in the country, and to do that through education, curriculum development, research, and community service,” Goodman says. A decade and a half after the program was started, “I feel we’ve accomplished that.” Goodman insists he was simply “turning the crank.” Essential encouragement and support have come from an ensemble of far-sighted mentors. They include Norman Altman, V.M.D., vice provost for research; Richard Bookman, Ph.D., associate dean, research and graduate studies; John G. Clarkson, M.D., senior vice president for medical affairs and dean; Lawrence Fishman, M.D., former chief of staff for research at the Miami VA Medical Center; Laurence Gardner, M.D., vice dean, chairman and professor in the Department of Medicine; Mark O’Connell, M.D., associate dean for medical education; Harvey Siegel, Ed.D., chair of the Department of Philosophy; and Steve Ullmann, Ph.D., vice provost for university administration.
The Ethics Programs are now a multidisciplinary, overarching, university-wide suite of programs that address ethical issues across professions such as medicine, law, and business, as well as social and policy issues. Research projects cover a wide range of topics, from hot-button issues such as stem cells, end-of-life care, and privacy, to information technology, environmental ethics, geriatrics, and evidence-based medicine.
“The idea is that you’ve got to teach doctors to know the latest evidence and to incorporate the best of it into their daily practice,” Goodman says. “There are zillions of journals out there and some research studies contradict each other. What is high quality? How can we systematically make the best science available to physicians? That’s what evidence- based medicine is, and it is now part of the School of Medicine’s curriculum.”
Nationally and internationally renowned, Goodman and the other faculty from the Ethics Programs, including co-director Anita Cava, J.D., associate professor of business law at the School of Business Administration, routinely advise legislators, collaborate on international research projects, write key texts, and lecture worldwide. Each year they collaborate with the Florida Bioethics Network (also directed by Goodman) on a Clinical Ethics Conference. The conference, which includes presentations from a variety of speakers, has also helped foster the Ethics Programs’ reputation as a center for high-quality ethics education. The Ethics Programs are currently being positioned to become one of only a handful of World Health Organization collaborating centers in ethics. “I first met with Dr. Goodman a few years ago when we were looking for strategic alliances,” says Fernando Lolas Stepke, M.D., director, Regional Program on Bioethics at the Pan American Health Organization. “The program had such a good reputation, and Dr. Goodman has published several important books.”
“The UM program has grown from a sort of sidewalk program down the hall to having recognition from the international community to help with issues and educational programs in international research ethics,” Goodman says.
Mapping the World’s Most Famous End-of-Life Case
![]() hile
Goodman was shaping UM’s Ethics Programs to academic acclaim, the
fate of Terri Schiavo was becoming increasingly public and complex. Goodman
watched the developments of the case closely. “There was something
different about this case,” Goodman says. His involvement with
the Schiavo case began when he gave an assignment to a student to create
a timeline, beginning with Schiavo’s birth, “and it hasn’t
ended yet. It didn’t end with her death in March 2005, it didn’t
end with her burial, and hasn’t ended after the governor tried
to get a prosecutor to look at it,” Goodman says. The timeline,
designed to be a resource for students and scholars, eventually became
the standard resource for people looking at the Schiavo case, including
different media. (The timeline and other Schiavo case resources are available
on the Ethics Programs Web site: http://www.miami.edu/ethics.)
hile
Goodman was shaping UM’s Ethics Programs to academic acclaim, the
fate of Terri Schiavo was becoming increasingly public and complex. Goodman
watched the developments of the case closely. “There was something
different about this case,” Goodman says. His involvement with
the Schiavo case began when he gave an assignment to a student to create
a timeline, beginning with Schiavo’s birth, “and it hasn’t
ended yet. It didn’t end with her death in March 2005, it didn’t
end with her burial, and hasn’t ended after the governor tried
to get a prosecutor to look at it,” Goodman says. The timeline,
designed to be a resource for students and scholars, eventually became
the standard resource for people looking at the Schiavo case, including
different media. (The timeline and other Schiavo case resources are available
on the Ethics Programs Web site: http://www.miami.edu/ethics.)
 |
||
The objectivity was key. “I think it’s clear what my opinion is—but I also think we’ve done a good job of keeping my opinion out of it,” Goodman says.
Which was invaluable to Jay Wolfson, the University of South Florida public health professor who had been appointed by Florida Governor Jeb Bush to be Schiavo’s guardian ad litem. Wolfson was required to represent Schiavo’s best interest in court, but he had no authority to make decisions for her.
He also had no knowledge of her case.
Goodman offered to help the beleaguered Wolfson, who had to digest the facts of the case, separate out the emotion, and try to determine the best course of action for Schiavo. “Ken was literally available 24/7 by phone and e-mail. He was a sounding board, a source of background material on the case and the issues,” Wolfson says. “He provided both substantive, technical/professional guidance, responses and advice, and personal support. He is, in the purest sense of the word, a skilled social scientist.”

After an emotionally wrenching month, on December 1, 2003, Wolfson concluded that Schiavo was in a “persistent vegetative state and unlikely to recover” —meaning her body functioned, but there was no cognition, self-awareness, or awareness of her surroundings.
But Schiavo’s percutaneous endoscopic gastrostomy tube, which provided nutrition and hydration, was not permanently removed until March 2005 (it had been removed and reinserted twice before then). Roughly two weeks later, Schiavo died.
In the time between Schiavo’s PEG tube removal and her death, Goodman spoke to 50 to 75 news organizations. While Goodman was happy that the school got the publicity, he was discouraged with the way the media covered the story.
A former journalist and computer researcher, Goodman knows about balanced coverage and the power of words.
“There was this weird notion that, in an attempt to be balanced, journalists had some duty to take the kooks seriously,” Goodman says. “So the only other side was represented for the most part by kooks. There were some credible sources of thoughtful opposition, but reporters didn’t find them. You had basically one of the most important end-of-life cases in history, and they’re giving equal time to a handful of extremists in the street outside the hospice. There are some cases in which ordinary ideas of journalistic balance serve us poorly.”
Goodman is currently editing a book about the Schiavo case, to be published by Cambridge University Press.
“There are nothing but lessons learned from the Schiavo case,” Wolfson says. “These relate to public education, professional education, and the education of policymakers. Getting medical students and law students together, getting physicians and attorneys to speak, and updating clinical information about good science and good medicine are all essential.”
![]()