
James Orovitz thought he was in the best
physical shape of his life. He was 60 years old and enjoyed
normal blood pressure and low cholesterol. Still, he
felt a little odd.
“I went to my family physician for my annual physical,
and I brought a list of symptoms with me,” says
Orovitz, whose complaints included slower and stiffer
walking, illegible handwriting, and a soft, hoarse voice. “I’m
the kind of person who smiles a lot, and it just felt
difficult to smile,” he says. His doctor diagnosed
Parkinson’s disease. A neurologist tested Orovitz
with a surprise backwards push. “I just lost my
balance totally,” Orovitz says.
The National Parkinson Foundation (NPF)
was there to pick him up. Another beneficiary of NPF
is Bernard J.
Fogel, M.D., now dean emeritus at the Miller School
of Medicine. Fogel’s personal connection dates from
the early 1960s, when he was serving as assistant dean
of medicine and recognized that his father was suffering
from Parkinson’s.
“Back then it was a pretty obscure disease,” he
recalls. “I would bring my father to the NPF, which
was adjacent to the medical campus, for treatment three
times a week.”
Fogel says his father’s regular visits made a big
difference. “The major thrust of his care consisted
of physical therapy and massages. But the consistency
benefited him in many ways beyond medication. It allowed
him social interaction with other people suffering from
the disease, he felt the therapeutic modalities were
very beneficial, and it permitted him to get out of the
house in an independent manner.”
Parkinson’s disease is a motor system disorder
that occurs when dopamine-producing brain cells die or
become impaired. It is named after James Parkinson, the
London physician who in 1817 was the first to describe
the disease in “An Essay on the Shaking Palsy.” Well
over a century later, in 1957 Jeanne C. Levey founded
the National Parkinson Foundation to help her husband
who suffered from the disease. In the 50 years since,
it has become the largest and oldest organization of
its type in the country.
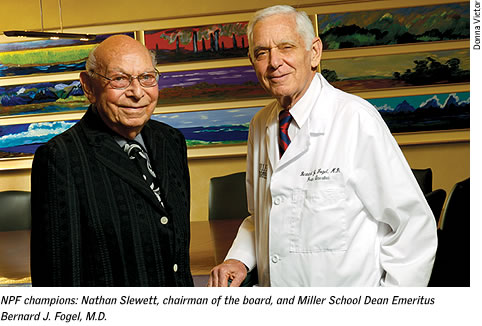
Levey nurtured the NPF until her death
at 92 in 1979, when the directors turned to board member,
businessman,
and attorney Nathan Slewett, who became president and,
later, chairman of the board.
The University of Miami’s relationship with the
NPF began at the same time through the efforts of Slewett,
Fogel, Harold Kravitz, Sidney Schreer, and Herb Zemel.
The partnership led to sharing of medical expertise and
emphasized patient care. “Under the terms of the
agreement,” says Slewett, “the medical school
moved the entire departments of neurology and neurological
surgery into the NPF building and agreed that these clinicians
and surgeons would be the ones to take care of all our
Parkinson’s patients. We also established a unique
clinic that provided physical, speech, occupational,
and recreational therapies, which became a national model.”
Perhaps most importantly, Slewett, who
at 94 years young continues his relationship to the institution
as a daily
volunteer, says, “It was also agreed that every
patient would be treated regardless of their ability
to pay.”
The foundation’s mission is threefold: to determine
the cause of Parkinson’s and ultimately find a
cure; to improve the quality of life of patients and
caregivers; and to educate the patient, their caregivers,
health care professionals, and the general public about
Parkinson’s disease and its treatment.
“The NPF’s relationship with UM was a giant
step in our history because it gave us credibility,” says
Slewett. “About three years after our partnership
started, the foundation created Centers of Excellence
that provided clinical care and outreach. We now have
54 centers all over the world.”
The centers are designed to act as regional “hubs” for
Parkinson’s disease research, care, education,
and outreach. They also offer innovative models of service
such as the Allied Team Training for Parkinson’s,
a one-of-a-kind interdisciplinary training program specifically
designed for allied health and nursing professionals
across the country.
“It’s unique because most training programs
have very little emphasis on Parkinson’s disease,
which is a very complex, idiosyncratic disease,” says
Ruth Hagestuen, R.N., M.A., director of field services
for the NPF in Miami. “We teach the cutting-edge
treatments in such areas as physical therapy and speech
pathology. These services, when delivered properly, can
make an enormous difference.”
When it comes to clinical care, the physicians
in the UM-NPF Division of Parkinson’s Disease and Movement
Disorders are at the forefront of diagnosing the disease,
setting up treatment, and developing appropriate therapies. “We
see patients in every stage of the disease,” says
Carlos Singer, M.D., professor of neurology and division
director.
Singer says that Parkinson’s does not just attack
motor skills. “For instance, sleep, diet, and depression,
gastrointestinal problems, and blood pressure problems
also arise. We try to establish if their symptoms are
linked to the disease or not.” He says that listening
to patients and helping them cope with the unknown is
key. “We acknowledge their fear and see if we can
allay it by reassuring them and educating them. Patient
education is very important because it empowers them.”
For some patients, surgery can also be
an option. Bruno V. Gallo, M.D., assistant professor
of neurology, and
Jonathan R. Jagid, M.D., assistant professor of neurological
surgery, use electrodes to perform deep brain stimulation.
A patient’s brain functions are measured to see
whether he or she would be a good candidate for surgery,
a procedure that modifies the behavior of the “trouble-causing” cells.
At any given time, Parkinson’s patients can take
advantage of dozens of clinical trials that are under
way to test new medications that are not yet publicly
available. Community outreach is also a big part of the
UM-NPF partnership. Nurse practitioner Angela Russell,
A.R.N.P., Ph.D., has a patient practice at Saint Catherine’s
Rehabilitation Hospital in North Miami. “This has
allowed us to establish contact in the community with
the purpose of focusing on the issue of treatment and
sharing information,” explains Singer.
For more than two decades, the Miami Brain
Endowment Bank housed at the NPF has worked on unlocking
the mysteries
of the human brain. Under the direction of Deborah
Mash, Ph.D., professor of neurology and the Jeanne C.
Levey
Professor of Parkinson’s Disease Research, the
bank is one of the nation’s largest collections
of postmortem tissue from patients who have willed their
brains to science. Researchers probe the tissue for clues
to the causes of brain-related disorders and diseases.
This vital center at the National Parkinson’s Foundation
is providing answers from a new frontier. “We’ve
long suspected an environmental link to these illnesses,
but now we think there is a complex interplay between
the genes and the environment,” says Mash, who
is now working closely with the acclaimed genetics team
that recently came from Duke University to the Miller
School. Margaret Pericak-Vance, Ph.D., has identified
genes critical to neurological illnesses. Her husband,
Jeffery Vance, Ph.D., M.D., chief of the Division of
Human Genetics, is a world leader in the genetics of
Parkinson’s disease.
Vance says conventional wisdom about the
disease has changed radically in recent years.
“James Parkinson, in his famous monograph describing
the disorder, considered that ‘lying on the damp
ground’ could
contribute to the development of Parkinson’s disease,” says
Vance. “While we consider this a bit humorous today,
the environment as the primary if not the only cause
of Parkinson’s disease was in favor until as little
as ten to 15 years ago.
 “Today we know that genetic mutations in several genes
[Parkin, Leucine Rich Repeat Kinase (LRRK2), a-synuclein,
PTEN-induced putative kinase 1 (PINK1), and DJ1] can
all cause Parkinson’s disease, each by themselves.
But these mutations represent only a small percentage
of the folks suffering from the disease. It is currently
the belief that most patients develop it through an interaction
between variations of certain genes and the environment.
This complex genetic picture is one which we are just
beginning to unravel.” “Today we know that genetic mutations in several genes
[Parkin, Leucine Rich Repeat Kinase (LRRK2), a-synuclein,
PTEN-induced putative kinase 1 (PINK1), and DJ1] can
all cause Parkinson’s disease, each by themselves.
But these mutations represent only a small percentage
of the folks suffering from the disease. It is currently
the belief that most patients develop it through an interaction
between variations of certain genes and the environment.
This complex genetic picture is one which we are just
beginning to unravel.”
It’s an exciting time for Parkinson’s research
and the NPF. Just ask James Orovitz. In the decade since
he began treatment, Orovitz—a generous NPF donor
who serves on the board of directors’ executive
committee—has been managing his illness with four
medications that have slowed the disease’s progress
so he can continue to play golf and “live a very,
very normal life.”
Orovitz partially attributes the successful
management of his disease to NPF’s support groups. “They
provide perspective—one day you may find someone
who is doing better than you, and the next day you might
find someone who is much worse. In the end you come to
the realization that you are what you are, and you accept
it and live with it. There are a lot of good days.” |