Mice who closely mimic
humans’ propensity to obesity and
diabetes inspired Keith Webster, Ph.D., to create a comprehensive,
cross-collaborative study “measuring just about everything
we can think of that is initiated by diet and ends up with
diabetes and congestive heart failure,” says the director
of the University of Miami Leonard M. Miller School of Medicine’s
Vascular Biology Institute (VBI). Helping to fund the basic
science study and hoping to translate these findings into clinical
applications
are Paul Kurlansky, M.D., of the Florida Heart Research Institute,
and Arthur Agatston, M.D., a voluntary associate professor
of cardiology who is better known as the author and creator
of the
South Beach Diet. “Diet studies are inherently very difficult
to do in humans,” says Agatston, one of the modern gurus
of dieting. “You can’t blind people to what they’re
eating.” Yet there is increasing concern in the medical
community about how what you eat can impact your health. And
there is fear that Americans are going to suffer the consequences.
That concern is well founded: According to the American Diabetes
Association, there are almost 21 million people, or 7 percent
of the population in the United States, who are estimated to
have diabetes. It is the fifth-deadliest disease in the United
States and the only major disease with a death rate that is
still rising. Cases of type 2 diabetes, which is associated
with older age, obesity, family history of diabetes, prior
history of gestational diabetes, impaired glucose tolerance,
physical inactivity, and race/ethnicity, have doubled in the
last two decades.
“Somewhere between 55 and 70 percent of the adult population—depending
upon whom you’re asking—is overweight in this country.
Somewhere around 20 to 25 percent of the adult population is
obese. That’s incredible. Obese is on the far end of
the spectrum—two standard deviations away from the norm.
Obesity predisposes one to type 2 diabetes and has, aside from
some of the obvious health risks, dramatic potential impact
on the incidence of coronary heart disease and congestive heart
failure. We’re only seeing the tip of the iceberg because
this trend toward weight gain has only happened over the last
20 years. Over the next 20 years, we’re going to see
the impact, the cumulative health impact, of having this problem,” says
Kurlansky, the director of research at the Florida Heart Research
Institute.
 Animal studies have been conducted in
the past to try to link diet and diabetes—to back up anecdotal evidence about
the harmful effects of a Western-style diet, which is high
in starch-type simple carbohydrates, with hard data. But the
mice used were leptin-deficient, meaning they lacked an adipose
tissue-derived hormone that signaled nutritional status to
the brain’s hypothalamus. These mice were “not
very good representatives of human disease,” Webster
notes. “Leptin-deficient mice tended to get very obese,
their diabetes lasted for a short time, and then they reverted,
whereas humans won’t revert back to a pre-diabetic state
unless they’re treated.” The new mice are much
more similar to humans who suffer from type 2 diabetes, who
are typically overweight but not necessarily grossly obese,
Webster says. “In many cases, people get insulin resistance
and the symptoms of type 2 diabetes before they get obese,
which is exactly what these mice do on a Western-style diet.” Animal studies have been conducted in
the past to try to link diet and diabetes—to back up anecdotal evidence about
the harmful effects of a Western-style diet, which is high
in starch-type simple carbohydrates, with hard data. But the
mice used were leptin-deficient, meaning they lacked an adipose
tissue-derived hormone that signaled nutritional status to
the brain’s hypothalamus. These mice were “not
very good representatives of human disease,” Webster
notes. “Leptin-deficient mice tended to get very obese,
their diabetes lasted for a short time, and then they reverted,
whereas humans won’t revert back to a pre-diabetic state
unless they’re treated.” The new mice are much
more similar to humans who suffer from type 2 diabetes, who
are typically overweight but not necessarily grossly obese,
Webster says. “In many cases, people get insulin resistance
and the symptoms of type 2 diabetes before they get obese,
which is exactly what these mice do on a Western-style diet.”
With his new mice, Webster is analyzing
the impact of the Agatston South Beach Diet on the obesity-related
impact on
type 2 diabetes.
Webster has two sets of mice, one of which is on a Western
diet (heavy on the mouse equivalent of cheeseburgers and
fries), while the other set of mice is on the South Beach
or Mediterranean-style
diet, where all their fat was derived from fish oil and starch
was reduced to a minimum. Both sets of mice are being fed
the same amount of food. The key elements of the South Beach
Diet,
which were laid out in Agatston’s bestselling book,
The South Beach Diet: The Delicious, Doctor-Designed,
Foolproof Plan for Fast and Healthy Weight Loss, focused on using good
fats along with good carbohydrates. Agatston created the
diet
initially to help improve the health of his patients, with
the accompanying weight loss being an unexpected bonus.
Agatston’s and others’ studies have shown that
eating “right” will have a positive impact on one’s
health. So it may seem that we already know what’s going
to happen to the sets of mice. But we don’t.
“Just recently, the Women’s Health Initiative
showed that a low-fat diet did not work to protect the heart,” Agatston
points out. “Science has gone beyond low-fat foods
to good fats and bad fats, but we’re checking into
the role of inflammation in this whole process.”
“Everything is out there in terms of what we expect, but nobody
knows exactly how obesity is related to diabetes. People
have some idea, but we don’t know,” Webster says.
Webster’s work will in part focus
on cytokines, which are small secreted proteins that mediate
and regulate immunity,
inflammation, and hema-topoiesis (the formation and development
of blood cells). Cytokines generally act over short distances
and short time spans and at very low concentration. They
bind to specific membrane receptors, which then signal the
cell
via second messengers to alter its behavior. Understanding
the signals that ping about the cellular level will help
scientists create appropriate responses for the body when
it hears the
wrong message.
“We know that obese tissue produces some dangerous cytokines,
but we don’t know how those dangerous cytokines make
a person insulin-resistant or hypoglycemic. And the reason
for doing these experiments in animals rather than humans—the
next phase is to do that in humans—is you can’t
take out the target tissue from a human study. So we will
be taking out skeletal muscle tissue, heart tissue, and adipose
tissue, and we will be looking at, in addition to the stem
cells, the molecular biology of that tissue and why is it
insulin
resistant,“ Webster says.
 Two things that aren’t known and that are really critically
important are the precise relationships between all those parameters
that need to be measured. The VBI will be looking at a panel
of up to 72 different cytokines, a massive increase from the
handful that other studies have examined. “We hope to
find which ones really respond to diet and which ones are really
related to the insulin resistance,” Webster notes. Two things that aren’t known and that are really critically
important are the precise relationships between all those parameters
that need to be measured. The VBI will be looking at a panel
of up to 72 different cytokines, a massive increase from the
handful that other studies have examined. “We hope to
find which ones really respond to diet and which ones are really
related to the insulin resistance,” Webster notes.
One of the most important of these cytokines
is called tumor necrosis factor alpha (TNF-alpha), and its
levels always
go up in inflammatory disease. “We think that this might
be the major signaling from obese tissue to mediate diabetes
and insulin resistance. We also think that these inflammatory
cytokines are floating around with the stem cells, and the
stem cells in the bloodstream are also communicating with the
stem cells in the bone marrow. These inflammatory cytokines
may be killing or modifying the stem cells so that they’re
not as good as the stem cells from a healthy mouse or a person,
and this may be at the root cause of the diabetes. This might
be why obesity and bad diet ultimately cause people to become
diabetic,” says Webster.
The second hypothesis being tested is
whether the stem cells themselves are causing most of the
damage. When you get a
defect in stem cells that are circulating, you end up with
a defect
in the repair processes that the stem cells are normally
doing. If you have adipose tissue producing dangerous or
inflammatory
cytokines that are destroying the stem cells, then they can
no longer repair the vessels. “Therefore, you get vascular
dysfunction, which can contribute to heart problems and a lot
of the problems that are associated with diabetes. The major
cause of death in the diabetic population is cardiac disease,
so you get vascular disease and then you get heart disease
and then you get heart failure—and this could all be
initiated by cytokine-related effects on the stem cells,” Webster
surmises.
“So we’re taking all these samples and doing all
these assays to see if we can reverse the diabetes—and
we think we can—and see if we can reverse the obesity—and
we think we can. And the key question is whether we can reverse
defects in the stem cells,” says Webster.
 “The important thing is that, from a medical point of view,
we need to understand what works, what doesn’t work,
why it works, and why it doesn’t work. So what this
project is attempting to do is to better understand obesity
on a very
physiologic, cellular level. The reason why we’re starting
in an animal model is because we’re dealing with very
complex processes here. In an animal model, you can control
many of the processes, and you can also adjust the time.
For a person to become obese, it may take 15 or 20 years.
For a
mouse to become obese, it may take four to six weeks in a
laboratory setting,” Kurlansky says. “The important thing is that, from a medical point of view,
we need to understand what works, what doesn’t work,
why it works, and why it doesn’t work. So what this
project is attempting to do is to better understand obesity
on a very
physiologic, cellular level. The reason why we’re starting
in an animal model is because we’re dealing with very
complex processes here. In an animal model, you can control
many of the processes, and you can also adjust the time.
For a person to become obese, it may take 15 or 20 years.
For a
mouse to become obese, it may take four to six weeks in a
laboratory setting,” Kurlansky says.
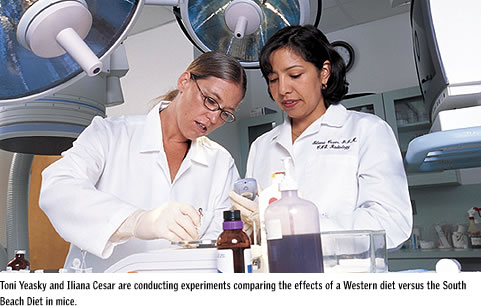
The first set of experiments in this program was initiated
early this year by VBI investigators Toni Yeasky, Iliana
Cesar, and Amber Wilson. The two groups of mice were maintained
on
their respective diets for 20 weeks, after which some of
the group 1 mice were switched to the South Beach Diet. Blood
was
drawn weekly and profiled for markers of type 2 diabetes,
body fat was measured by X-ray scanning, and plasma cytokines
were
measured by antibody microarray. Leopoldo Raij, M.D., professor
of medicine and an internationally acclaimed expert in hypertension,
will monitor blood pressure parameters of the mice during
dietary regimes. At selected time points, stem cells were
isolated
from bone marrow and cultured.
The Western diet group 1 mice were extremely insulin resistant
and hyperglycemic at ten weeks and displayed multiple signs
of type 2 diabetes. They tended to sleep more and move around
a lot less. At 20 weeks, some of these mice began to display
evidence of liver damage.
In contrast, the South Beach group 2 mice
had normal glycemic levels and were healthy with no signs
of diabetes even at
20 weeks. Group 1 mice that were switched to the South Beach
Diet
showed clear signs of improved insulin sensitivity and glycemic
control after six weeks. An extremely novel finding was that
insulin resistance correlated very closely with an accumulation
of the inflammatory cytokine monocyte chemoattractant protein-1
(MCP-1), but not with tumor necrosis-a (TNF-alpha) or interleukin-6.
The latter two cytokines are widely believed—but not
proven—to be responsible for insulin resistance.
Another finding was that the group 1 mice had significant
myocardial hypertrophy (heart enlargement) that increased
progressively
to 20 weeks.
Stem cells were taken from the bone marrow of diabetic group
1 and healthy group 2 mice. These cells are currently under
culture, and preliminary indications are that cells from
the diabetic mice are growth retarded.
The second group of mice in the study are already at 20 weeks.
These mice will be used exclusively for stem cell isolations
and tissue collections. “We will culture stem cells from
tissues isolated from extremely diabetic and normal, healthy
mice, as well as mice in which the diabetes has been reversed.
These cells will be examined for gene expression by microarray,
cytokine production, growth, and differentiation. We expect
to find differences in these cells that could be linked to
the role of diabetes in heart disease as well as the link between
obesity and diabetes,” says Webster.
“What’s really important in all of these experiments is to see if
you can reverse the process. This study may not answer that, but it might give
some insights,” Kurlansky says.
The Florida Heart Research Institute and South
Beach Diet Doctor Arthur Agatston are confident that this
comprehensive study is going to give hard science
answers to some clinically related questions. They’ve both given $100,000 each
to fund the early phases of the research, but Agatston says he’s planning “on
committing to this research for the long-term.
“I think we’re going to find the key to a lot of diseases, not just
vascular.” |
|