 The deadly medical mystery that rocked Panama
last September began innocuously, with a trickle of patients
complaining of
weakness and tingling in their legs. Within a matter of weeks
Panama was grappling with a health crisis that claimed scores
of lives until inspired sleuthing by a University of Miami-trained
physician brought the dying to an end. The deadly medical mystery that rocked Panama
last September began innocuously, with a trickle of patients
complaining of
weakness and tingling in their legs. Within a matter of weeks
Panama was grappling with a health crisis that claimed scores
of lives until inspired sleuthing by a University of Miami-trained
physician brought the dying to an end.
Nestor Sosa, M.D., brilliantly fulfilled the
promise that gained him entry into the Miller School’s prestigious William
J. Harrington Medical Training Programs for Latin America, currently
celebrating its 40th anniversary. A Harrington trainee in the
late 1980s, Sosa “was one of our best and brightest,” says
Mark Gelbard, M.D., associate professor of medicine.
Sosa, 45, has received international acclaim
for discovering that diethylene glycol, a poisonous substance
used in antifreeze,
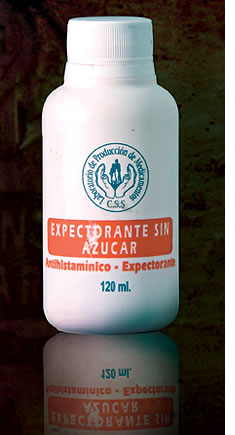
was unwittingly mixed into 260,000 bottles of Panamanian cough
medicine. The diethylene glycol was manufactured in China,
where it had been labeled 99.5 percent pure glycerin, a sweet
compound
used in foods and drugs. Both substances are sweet-tasting
and viscous.
Prior to the deaths in Panama, unscrupulous
Chinese businessmen had knowingly substituted diethylene glycol
for more expensive
glycerin in other
countries, with deadly results.
That wasn’t on Sosa’s mind in September, when patients
experiencing weakness and tingling in their legs began showing
up at the Panama City hospital where he worked as an infectious
diseases specialist. The facility, Caja de Seguro Social/Complejo
Hospitalario Metropolitano, is part of Panama’s social
security system. Sosa was asked to investigate the malady, which
medical researchers had erroneously identified as Guillain-Barré syndrome,
a rare neurological disorder.
That’s because the initial stages of diethylene glycol
poisoning mimic Guillain-Barré syndrome, an often fatal
autoimmune disease with no known cause or cure. But Guillain-Barré was
quickly ruled out when the patients in Panama began to also suffer
kidney failure. By early October the death toll was in the low
teens before eventually peaking at a reported 426 fatalities.
In the midst of a desperate search for a killer,
Panama’s
Health Ministry declared a national epidemic. Sosa notified officials
at his hospital that the mysterious malady was killing roughly
half its victims, and the Panamanian government asked him to
establish and lead a medical task force.
Because 19 of the 21 patients who came to his
hospital were older men, Sosa wondered if aphrodisiacs might
be behind
the deaths.
But that hunch didn’t pan out. Most of the deceased were
over 60 and suffered from hypertension and diabetes. Half had
been taking a blood pressure drug called lisinopril, so as a
precaution Panamanian pharmacies were banned from dispensing
the medication. However, tests showed the drug to be safe.
Sosa’s tenacity finally began to bear fruit following the
admission of a heart attack victim to his health care facility.
While hospitalized, the patient came down with the mysterious
ailment.
“It was obvious that whatever was causing
his problems had to be on the medication list,” Sosa
says.
The patient had been administered several drugs,
including lisinopril. One of its potential side effects is
a persistent
cough. A short
time afterward, Sosa heard of a patient in a private Panamanian
hospital who’d presented Guillain-Barré symptoms
after being given lisinopril.
 “What really broke the case was when Nestor
heard about that patient who wasn’t in the social security
system,” says Gordon
Dickinson, M.D., professor of medicine and chief of infectious
diseases at the Miller School. “When that patient showed
up, Nestor jumped in his car and went to interview this patient
in another hospital.” “What really broke the case was when Nestor
heard about that patient who wasn’t in the social security
system,” says Gordon
Dickinson, M.D., professor of medicine and chief of infectious
diseases at the Miller School. “When that patient showed
up, Nestor jumped in his car and went to interview this patient
in another hospital.”
While there, he noticed a half-empty bottle
of cough syrup issued through the social security system. “He didn’t belong
to the social security health care system, but he wanted to save
money, and the syrup was free,” Sosa recalls.
On October 10, 2006, Sosa arranged for several
bottles of the cough syrup to be flown to the United States,
where they
were
analyzed by the Centers for Disease Control and Prevention
in Atlanta. The following day, United States health care
officials informed Panama that the cough syrup had been contaminated
with
diethylene glycol.
Successfully tracking down the killer that terrorized
Panama filled Sosa with mixed emotions. “I was happy because we
found the cause, and we knew that was the beginning of the end,” he
says. “On the other hand, we knew it was something we had
manufactured, that had actually been made in a lab in my hospital.”
The Panamanian cough syrup tragedy triggered
an uproar among a citizenry already furious with a social security
health
care system infamous for not having enough medication and
long waiting
lists for surgeries.
“This was a major blow to the social security
system,” Sosa
says. “There is an investigation going on that’s
not finished, along with a public outcry to take out the
minister of health. Because of the notoriety from this I
got another job.”
After working for Panama’s social security health care
system for 14 years, on April 1 Sosa took a position training
Central American health care workers. Panama’s social security
system claims 79 people died and 119 were affected by the adulterated
cough syrup. The Panamanian district attorneys’ office,
however, puts the death toll at 426.
Sosa’s role in identifying diethylene glycol as a mass
killer is the crowning achievement thus far in a life marked
by an uncompromising quest for excellence.
Born in Camaguey, Cuba, Sosa and his family
moved to Panama when he was 9. He enrolled in the University
of Panama in
1980 and
graduated six years later with a medical degree. A knack
for chess resulted in him being named a national master of
chess
in 1982 and national chess champion of Panama the next year.
Following graduation from the University of
Panama, Sosa completed an internship at his former place of
employment,
Caja de Seguro
Social/Complejo Hospitalario Metropolitano, followed by a
month-long clinical rotation at the Copenhagen Komune Hospital,
where
he focused on internal medicine.
Thinking several steps ahead, like the chess master he is,
Sosa thought it would be useful to train at UM under the
auspices of The William J. Harrington Medical Training Programs
for
Latin
America.
Sosa did three years of residency training followed by a
two-year fellowship in infectious diseases. Gelbard, who
directed the
Harrington residency program when Sosa attended, recalls
that he “was curious and had a thirst for knowledge.”
Attributes that would save untold numbers of
Panamanian lives.
|