
She’s 12, wears her long hair in neat cornrows, and
already has some serious risk factors for cardiovascular
disease—high blood pressure, high cholesterol, and
too many extra pounds from a sedentary lifestyle and high-fat
diet. “There aren’t any kids in my
neighborhood, so I’ve just been watching a lot of
TV and eating stuff that’s really bad for me,” says
Angela, the Miami-Dade County sixth grader who is participating
in a research program at the Miller School of Medicine’s
Department of Pediatrics. She is learning how to exercise
more and eat better. About one-third of the nation’s
children and adolescents are overweight or obese, and for
some minority groups the rate is much higher. Since obesity
is considered the second leading cause of preventable disease
and death in this country—second only to tobacco
use—hundreds of thousands of children are facing
an uncertain future. “We have a whole generation
of kids who for the first time may not live as long as
their parents,” says Steven Lipshultz, M.D., chair
of pediatrics and associate executive dean for child
health, who has assembled a diverse team of clinicians
and researchers
to try to change that. The team literally is writing
the book on assessing and preventing cardiovascular risks
in children, having been asked by the American Academy
of Pediatrics (AAP) to contribute chapters on preventive
cardiology, high blood pressure, and heart failure to
the AAP textbook on pediatric primary care.
“This is the very first AAP textbook
on pediatric primary care, and they asked us because
we’re recognized
as being really unique in the country,” Lipshultz
says. “There are very few places that are trying
to document not only how significant cardiovascular risk
is at a young age, but to come up with interventions
that make a difference.”
UM has one of the largest cardiac rehabilitation
programs for children and a team of people who specialize
in cardiology,
nutrition, psychology, gastroenterology, epidemiology,
exercise physiology, and endocrinology—all working
together as a group. “It’s a multifactorial
set of issues that require a multidisciplinary approach,” Lipshultz
notes.
In addition to its work on weight and
obesity, the team also is working on prevention of other
cardiac risk factors,
including exposure to secondhand smoke.
“Certainly the risks are higher than they used to be,” says David
A. Ludwig, Ph.D., professor of pediatrics and epidemiology and public health,
whom Lipshultz calls “among the best in the country at assessing childhood
risk and prevention.”
 Although experts speculate that the long-term
effects of obesity and other cardiovascular risk factors
in children will have dire consequences later in life,
Ludwig feels
ongoing research is essential. “At present, definitive longitudinal data
supporting such speculations is limited.” Although experts speculate that the long-term
effects of obesity and other cardiovascular risk factors
in children will have dire consequences later in life,
Ludwig feels
ongoing research is essential. “At present, definitive longitudinal data
supporting such speculations is limited.”
Ludwig, who serves as biostatistician
and designer of studies to assess risk, came to the University
in March from the Medical College of Georgia, where he
was co-director of the Georgia Prevention Institute.
“There are an incredible number of issues here. Kids are not getting as
much exercise,” he
says. “They’re not involved as much in free play as was the case
20 or 30 years ago due to the way neighborhoods are structured now. They’re
more likely going to an organized sport like soccer, and if they’re not,
they’re in front of the TV.
“One of the biggest culprits is
the availability of cheap fast food. We actually have
a surplus of food in this country, and when it comes
in the form of fast
food, it’s very inexpensive and high in calories and fat.”
Preventing obesity during childhood is
critical, because habits formed early often last a lifetime.
Research has shown that overweight adolescents have up
to an 80 percent chance of becoming overweight or obese adults, and earlier
onset
of obesity leads to the earlier onset of related illnesses, such as type 2
diabetes, heart disease, stroke, and certain types of
cancer.
About 18 percent of children in this country
are obese, up from 5 percent in 1974, according to a
study published over the summer [June 27] in JAMA, the
Journal
of the American Medical Association. An estimated 60 percent of obese children
between the ages of 5 and 10 have at least one risk factor for heart disease,
the leading killer in the United States, and 20 percent have two or more risk
factors, the JAMA report said.
A number of previous studies at UM and
elsewhere have shown that African-American and Latino
children living in low-income communities are at greatest
risk for
obesity and related health problems. The American Heart Association has issued
a scientific statement saying overweight children and adolescents represent
one of the most important current public health issues
because of the related medical
complications.
In June a committee of health professionals
issued recommendations saying doctors should assess children’s weight and height annually and attempt to treat
overweight kids based on their age, body mass index (BMI), and any related medical
conditions. BMI is a number calculated from a person’s weight and height
and, in general, reflects how much body fat the child has. The AAP, which participated
in the committee’s work, said while there is a lack of research on the
long-term impact of treating overweight children, doctors should still make it
a priority.
“The enormity of the epidemic necessitates this call to action for pediatricians
using the best information available,” the AAP said.
Childhood onset of metabolic syndrome,
which is diagnosed by testing fasting insulin and glucose,
systolic and diastolic blood pressure, and cholesterol
and
triglyceride levels, significantly increases the risk for type 2 diabetes and
cardiovascular disease.
Sarah Messiah, Ph.D., M.P.H., a research
assistant professor in pediatrics and an epidemiologist,
was involved in a study that assessed the prevalence
of the
metabolic syndrome in a clinical sample of 225 children ages 3 to 18. Reflective
of South Florida, the children were largely from minority backgrounds: 66 percent
Hispanic, 24 percent Afro-Caribbean/black, 5 percent white, and 5 percent multiracial.
“We found metabolic syndrome in
20 percent of this clinic sample,” Messiah
says. “The youngest child was only 7 years old. Those kids who were morbidly
obese were four times as likely to have the syndrome compared to kids of normal
weight.”
And the risks for disease are showing
up in younger and younger children.
Messiah and colleagues in another study
looked at 302 children ages 2 to 5 from eight preschools
in Miami-Dade County. Overall, 30 percent of the children
had
a BMI greater than the 85th percentile, which is about 4 percent higher than
the rest of the country. Within some groups of Hispanic children, 39 percent
exceeded the 85th percentile.
During the research, parents were involved
to some degree, she says. “We’d
do a cooking night and they would bring recipes from their ethnic background.
The goal was to keep the ethnicity intact, but make it healthier or as healthy
as possible,” Messiah says.
“Cultural sensitivity is critical to trying to be able to manage this and
educate
people at the earliest stages,” Lipshultz adds.
Alan Delamater, Ph.D., director of clinical
psychology and professor of pediatrics, is working with
overweight third and fourth graders at two Miami-Dade
schools
and their parents on a one-year demonstration program. “The work is focused
on metabolic syndrome, which really is a risk for both type 2 diabetes and cardiovascular
disease,” he says. “We’re using the schools as a site because
people are more likely to take part. You can’t expect the working-class
families we’re working with to travel across town to a medical center.”
The study groups are divided into two
comparison groups of 16 or 17 children and their parents. “The more intensive group gets multifamily group meetings
at the school and several individual meetings at the family home,” Delamater
says.
In a small pilot project with five families,
he found them to be cooperative and accepting of ideas
to improve their children’s health. “The parents
and kids both did better, and they’re very responsive and open to having
team members come into the house, sit at their kitchen table, look in their refrigerator,
and talk about what they’re feeding their kids,” he says.
Delamater is collaborating with Sheah
Rarback, M.S., R.D., a registered dietitian and director
of nutrition at the Mailman Center for Child Development
in the
Department of Pediatrics. “With any program, the involvement of the family
is really critical,” Rarback says.
Rarback, who sees overweight children
in her daily practice, explains that just telling children
about the serious diseases they may face in the future
if they
don’t adopt a healthier lifestyle does not bring about the needed change.
“Fear doesn’t work very well. It doesn’t even work with adults.
If
I have a 26-year-old in my office and say, ‘If you don’t lose weight,
you’re going to be diabetic by the time you’re 40’, it doesn’t
work,” she says. “When do they change? When they have the heart attack,
not ten years before they have the heart attack.”
Delamater and Rarback also have another
project with the school system involving 5- and 6-year-olds—not just overweight kids, but all kids. The purpose
of this project is to test the feasibility and efficacy of a school-based, multicomponent
intervention to prevent metabolic syndrome.
“Part of the program will utilize
SPARK (Sports, Play and Active Recreation for Kids),
based in San Diego. They have a whole lot of gadgets
and toys, jump ropes
and things, that can help the teacher get the kids up and moving during the
school day, and that is fun for them,” Delamater
says.
The increase in the youngsters’ physical activity is coupled with creating
a social environment within the schools that emphasizes and values healthy lifestyles.
Other components are based on a tool developed by the Centers for Disease Control
and Prevention called the School Health Index, which schools can use to improve
physical activity and encourage healthy eating, as well as prevent tobacco use,
accidental injuries and violence, and control asthma in students who have the
disease. The CDC makes copies of the program available to schools for free.
“Our approach is to work with the principal, the administration, the staff,
the
food-service people,” Delamater explains. “We have a planning grant,
and we’re going to develop the program in one school and have a comparison
school, working with 60 kids in each school.”
South Florida’s richly diverse population also has given researchers the
chance to break new ground studying a Haitian population largely ignored in the
past. Nancy Stein, Ph.D, M.P.H., an epidemiologist and research assistant professor
in pediatrics, is finding they have their own unique set of health issues.
“They may not have anything in common [with other black groups] other than
the
color of their skin,” says Stein, who, along with UM colleagues, has done
the first studies on the Haitian population and is applying for grants to do
more.
Stein says a first step in research is
often to do a medical chart review and collect information
that may generate hypotheses for future funded research.
She says that Lipshultz and Tracie Miller, M.D., director of the Division of
Pediatric Clinical Research in the Department of Pediatrics, both encouraged
her to pursue the research.
“We know that overweight and obesity is everywhere but much higher in the
minority populations. I thought Haitian kids were going to be different because
they all looked thin to me,” Stein says. “But I was shocked, really
surprised, that once they come here they gain weight very quickly, about 4 percent
per year, and in no time it’s the same as if they had lived here forever.
“The bottom line is they gain weight, and that puts them at risk for cardiovascular
disease and other diseases. It shows that the time to intervene is when they
come here. And that’s what we’re going to do next.”
Stein and colleagues are working with
UM’s Center for Haitian Studies to
set up a pilot program to try to prevent young Haitian newcomers from joining
their American counterparts in becoming overweight. Stein says Haitian families
have a complex set of issues that may make it difficult to live a healthy lifestyle.
“These are not the parents who are
staying home and making sure their kids eat well after
school. They’re holding two and three jobs; they’ve
got double minority status; they speak Creole but many
don’t read Creole, so
it’s not a matter of handing them a pamphlet to study.”
Stein found that Haitian adults who immigrate
to the United States weigh 10 to 15 percent less than
average Americans and may close the gap over about ten
years
time. “But for kids, that time element isn’t there. They get immersed
in the whole culture very rapidly.”
Miller, a pediatric gastroenterologist
and professor of pediatrics, says once research shows
results in bringing kids back from the brink of obesity
and all
of its inherent risks, the next hurdle is getting insurers to pay for such
a program. Her research shows that a 12-week active intervention
program, counseling
kids on the importance of a healthier diet coupled with a structured fitness
program, produces results.
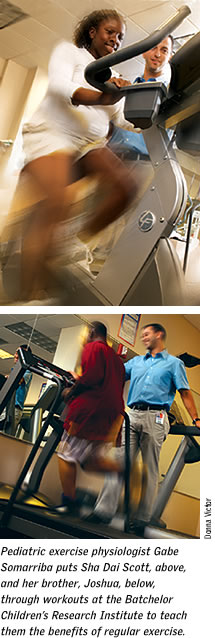
“Our pediatric exercise physiologist, Gabe Somarriba, in the Division of
Pediatric Clinical Research, works with the children twice a week for an hour
and a half,
using aerobic training on a stationary bike, the treadmill, and with weights,
and ellipticals, and as they get stronger he gets them to do more,” Miller
says.
On a recent morning in the gym at the
Batchelor Children’s Research Institute,
Somarriba was putting Angela through an individualized workout. He works with
children as young as 6. They each get baseline blood work, bone density scans,
and other tests that are repeated at three- and six-month intervals to measure
progress.
During the last two weeks of the 12-week
intensive program, Somarriba begins to teach them how
to continue to work out at home and sends them out with
some
dumbbells and a Thera-Band, a stretchy elastic band they can use for resistive
exercises. During the three months the kids are working on their own, he calls
them to provide encouragement and to see how they’re doing. After the three
months, Miller brings them back in to reassess their progress.
“We’ve gotten some good data to show the kids do really well in the
first
three months, and most continue to improve at home but not as dramatically.”
Miller wants to expand the program to
bring in kids from the community whose parents are willing
to pay out of pocket for it. She started talking to HMOs
about six years ago to try to get them to buy into the idea of covering such
a program, but to no avail.
“I keep hoping that with all the focus now on childhood obesity, they will
change
their attitude. I’m trying to prove this would save them money in the long
run,” she says, “but unless you’ve had a heart attack, they
won’t pay for a program such as this that may actually prevent the child
from having the heart attack.”
Nancy McVicar is a freelance writer living in South Florida.
She has been writing about health and medicine for
18 years.
|