|
 |
ARRA Apparent
By By Maya Bell | Photo By John Zillioux
NIH grants awarded through the $787 billion American Recovery and Reinvestment Act are funding Miller School studies that seek bench-to-bedside breakthroughs in many important biomedical disciplines
 |
| Maria Abreu, M.D., professor of medicine and chief of gastroenterology, shown here with, left, research associate Cecilia España and, right, Rebeca Santaolalla, Ph.D, received $362,000 to study the role of immune-system responses to intestinal microbes in colorectal cancer. |
The worst economic slump since the Great Depression is exacting a terrible toll. But amid the grim news of lost jobs, homes, and health insurance, seeds of hope are being planted for medical breakthroughs as varied as curing colon cancer, reducing diabetic amputations, restoring lost vision, and limiting brain damage after traumatic injury.
The seeds are sprouting in the labs of Miller School faculty members who so far have won 82 grants worth $49.1 million over two years to pursue research priorities of the National Institutes of Health (NIH) that hold the promise of improving the lives of millions of people.
The $787 billion American Recovery and Reinvestment Act (ARRA) that President Obama pushed through Congress to mend the economy included $8.2 billion for the NIH. The agency and its 27 institutes and centers are using the funds to accelerate ongoing or kick-start new research projects that could stimulate the economy and quickly produce high-impact breakthroughs.
Racing against extraordinary deadlines, Miller School faculty responded impressively, submitting 430 grant applications for a total of $382 million. Of the 82 grants awarded to date, 11 came in two new, highly competitive categories: Challenge and Grand Opportunities, or GO, grants. That’s no small feat considering that Challenge Grants alone attracted 20,000 applications nationwide. Equally impressive, three Miller School faculty received two of the 31 GO grants awarded by the National Human Genome Research Institute (NHGRI).
“That is extraordinary,’’ says Richard Bookman, Ph.D., vice provost for research and executive dean for research and research training. “Just a couple of years ago, UM wasn’t getting any NHGRI funding.’’
Eden Martin, Ph.D., director of the Center for Genetic Epidemiology and Statistical Genetics, received one of the NHGRI grants—$1 million over two years—to develop statistical methods for next-generation sequencing in disease association.
The team of Stephan Schurer, Ph.D., research assistant professor of molecular and cellular pharmacology, and Vance Lemmon, Ph.D., professor and Walter G. Ross Chair of Developmental Neuroscience, received the other, for $1.5 million, to develop an ontology for chemicals of biomedical interest.
Overall, Lisa Metsch, Ph.D., professor of epidemiology and public health, received the Miller School’s largest stimulus award—$12.3 million over two years. To be shared with the San Francisco Department of Health, the grant will fund a study of the effectiveness of HIV-prevention counseling by following 5,000 patients in nine clinics for sexually transmitted diseases.
Other grants, both large and small, are enabling Miller School faculty to forge new frontiers in fields ranging from stroke prevention to breast cancer. Among these promising projects are those profiled below.
Protecting Injured Brains
Imagine this: One of the 1.4 million Americans destined to suffer a traumatic brain injury this year is rushed to the Ryder Trauma Center, where doctors administer a new drug, halting the death of the patient’s brain cells, protecting cognition, and reducing the risk of post-traumatic epileptic seizures.

|
| W. Dalton Dietrich, Ph.D., scientific director of The Miami Project to Cure Paralysis, received an NIH grant to study neuron death in traumatic brain injury and a new compound that may offer neuroprotective benefits and improve outcomes for patients.
|
For W. Dalton Dietrich, Ph.D., scientific director of The Miami Project to Cure Paralysis, the scenario is no fantasy. It’s the goal of the $903,771 Challenge Grant that he, along with Helen Bramlett, Ph.D, associate professor of neurological surgery, and Thomas Sick, Ph.D., professor of neurology, received to determine if traumatic brain injury (TBI) activates necroptosis, a newly recognized pathway for neuron death. If it does, they’ll also test a new compound that may protect the brain from further damage.
“After brain trauma, all neurons at risk do not die immediately,’’ Dietrich explains. “They die over hours, days, and weeks, so you may have a window of opportunity to give a neuroprotective drug to stop cell death. We hypothesize that reduction of cell death will improve cognition and reduce the incidence of post-traumatic epilepsy.’’
Post-traumatic epilepsy is a debilitating consequence of TBI, affecting 30 percent of patients who suffer moderate or serious brain insults, usually from car accidents, violence, athletic mishaps or, in increasing numbers, bomb blasts. TBI is the hallmark injury of U.S. soldiers serving overseas.
But TetraLogic Pharmaceuticals is giving them new hope. The firm has developed a small peptide that may inhibit the molecular mechanism that triggers progressive neuron death. The Pennsylvania-based company is collaborating with The Miami Project to study necroptosis and test the new compound in the project’s brain trauma model, one of the best in the world.
If Dietrich and colleagues prove the compound saves neurons and decreases post-traumatic epilepsy in animals, he says it could be tested on humans and eventually make its way to emergency rooms across the country.
“It’s very exciting,’’ he says. “Right now we don’t have a lot to offer people with brain trauma to limit secondary cell death and its consequences.”
Combating Colon Cancer
Ask Maria Abreu, M.D., professor of medicine, chief of gastroenterology, and a leading authority in inflammatory bowel disease, why she chose her specialty and she makes a joke: “Because it’s very glamorous!”
|
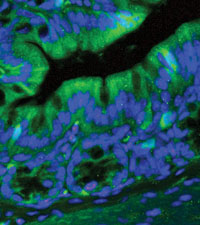
| This stained microscope image of a transgenic mouse colon used to study the role Toll-like receptors play in colon cancer has been magnified 400 times.
|
Though gut bacteria are, of course, anything but glamorous, Abreu believes intestinal microbes—specifically the innate immune system’s reaction to them—may be key to preventing or curing colon cancer, the third most common cancer in the United States.
NIH grant reviewers think she’s on to something. They awarded her $362,000 in stimulus funds for one year, with the likelihood of more down the road.
“Our colons are full of bacteria, and we believe colon cancer occurs in part because the immune system in our gut recognizes and overreacts to these bacteria and, over time, causes inflammation,” Abreu says. “We know inflammation promotes colon cancer. We want to see if innate immune signaling in the intestine is the cause.’’
A continuation of a grant Abreu brought from Mount Sinai Medical Center in New York, where she directed the Inflammatory Bowel Disease Center, the money allows her five-person lab to advance her groundbreaking research on Toll-like receptors (TLRs) into a new realm.
Previously she pinpointed how TLRs, molecules that alert the immune system to the presence of microbial infections, are normally expressed in the intestine. Now she’ll be able to explore preliminary data that shows a specific receptor, TLR4, is over-expressed in most sporadic colon cancers and promotes tumors.
The long-term implications could be significant for the 50,000 Americans destined to die every year from colorectal cancer. That’s because the next step would be trying to prevent or treat colon cancer by blocking TLR4.
“The stimulus package came at a great time,’’ Abreu says. “We are using the money to keep technicians and scientists at the bench, working on this important discovery.’’
Teasing Out Tissue Secrets
Central nervous system cells don’t regenerate after injury, and scientists who hope to figure out how to repair or replace them face an obstacle in the lab.

|
| Jeffrey Goldberg, M.D., Ph.D.
|
When they culture brain, spinal cord, or retinal cells, they can’t really replicate how the cells develop, function, and operate in response to injury because they’re lying in a dish, not tethered to their natural three-dimensional environment.
But Jeffrey Goldberg, M.D., Ph.D., assistant professor of ophthalmology at the Miller School’s Bascom Palmer Eye Institute, plans to use his $764,972 Challenge Grant to build the first three-dimensional model for studying neural tissues in a culture dish, and he’ll start with the retina. His goal is to re-create the light-sensitive lining of the eye from its basic cell types, layer by layer, on a polymer gel scaffold less than a millimeter thick.
“The retina is a great place to start with a model for the brain, or the nervous system in general, because the retina has this very ordered structure of layers of different cells,’’ Goldberg explains. “So, we can make one layer of one retinal neuron and put that right next to another retinal neuron—similar to the real retina.’’
Stem-cell experiments with the 3-D retina model may help scientists better understand neural development, integration, and communication, leading to more effective treatments for degenerative eye diseases like glaucoma. The hope, though, is they’ll also pave the way for whole tissue replacement therapies throughout the nervous system.
“This is a first step toward tissue engineering,’’ Goldberg says. “Instead of replacing just one cell or cell type in a damaged retina, or in a stroked-out section of the brain, we’d like to build the whole missing tissue.’’
Avoiding Amputation
More than half the chronic foot ulcers that often develop in people with diabetes fail to heal, leaving doctors little choice but to amputate a toe, a foot, or even a leg to save remaining healthy tissue. As a result, diabetics suffer a lot of amputations—about 82,000 a year in the United States alone. “It is astonishing: There is a worldwide statistic that says every 15 seconds a foot or part of the leg is being amputated due to a diabetic foot ulcer,’’ says Marjana Tomic-Canic, Ph.D., professor of dermatology and director of the Miller School’s wound healing and regenerative medicine research program. “This is a huge issue.’’

|
| Marjana Tomic-Canic, Ph.D., professor of dermatology and director of the Miller School’s wound healing and regenerative medicine program, discusses her study with research fellow Elizabeth Lebrun. The study seeks to develop a quick test physicians could use to identify non-healing diabetic foot ulcers that require earlier, more aggressive treatment. |
But thanks to a $902,641 Challenge Grant Tomic-Canic and her lab received, she envisions a day when doctors will use an on-the-spot test to distinguish foot ulcers that have lost the potential to heal when treated with standard therapies from those that still have the ability. By expediting more aggressive biological treatments for non-healing wounds, the innovation could save limbs and improve the lives of millions of diabetics.
But first, Tomic-Canic must prove her theory and confirm preliminary findings that cells on the edges of non-healing ulcers include one or two proteins that aren’t present in healing wounds. She’s already identified the possible biomarkers and will use the grant to collect tissue from 50 patients with ulcers at UM and New York University to test for the proteins and their correlation to non-healing outcomes.
She is confident that can be accomplished in the next two years, leading to immediate changes in treatment strategies in wound centers across the country and paving the way for a future instant test that can distinguish healers from non-healers.
“It’s very exciting,’’ she says. “As a molecular biologist, you don’t often have a chance to bring a basic science discovery to the bedside.’’ |
 |
 |