|

On the suburban campus of Florida Atlantic University in Boca Raton, a small group of students armed with a mountain of research is comparing notes and engaging each other to find a solution to a medical problem. From the eager conversation, myriad charts, busy fingers on laptops, and the pleased expression of Miller School clinical professor Daniel M. Lichtstein, M.D., these first-year medical students have come up with responses to a complex set of questions surrounding a case of hemophilia.
With this one carefully crafted problem, these Miller School students—part of the first class that will obtain UM medical degrees while studying all four years on the Boca Raton campus—have covered several basic science topics, aspects of the doctor-patient relationship, and medical ethics. And being a small sub-group of eight in the freshman class of only 32 students, they are getting to intimately know each other and the faculty. They’ll also be able to see how doctors perform in the real world very early in medical school, through a cutting-edge program that gives them a heavy dose of exposure to physicians, hospitals, and patients, starting in the first semester.
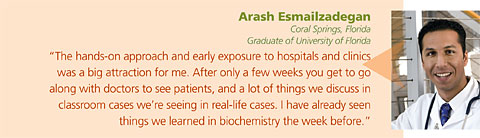
“We’re not only learning science, but we’re learning to be effective physicians from the start,” says Arash Esmailzadegan, a freshman from Coral Springs who received his undergraduate degree from the University of Florida. “There is a strong focus on catering to students’ needs while preparing us for what’s going on in medicine right now. There are a lot of hands-on approaches to things, and we’re able to go to class, learn the sciences, and learn their applications simultaneously.”
Though the private University of Miami and the public Florida Atlantic University joined forces to create the historic Miller School of Medicine at FAU (UMMSM@FAU) in 2004, this year the partnership took big steps forward, not only to extend the two-year studies to four (previous classes completed the final two years at the Miami campus), but to form stronger ties with local physicians, community hospitals, and the Palm Beach County Health Department.
“The Miller School has had a long history of dedication to innovative medical education and advanced patient care, and we’re proud to be extending our tradition to our first regional campus,” says Pascal J. Goldschmidt, M.D., senior vice president for medical affairs and dean of the Miller School. “We’re committed to strengthening our partnership with FAU, the hospitals, and the community to produce more high-caliber doctors to meet the needs of the county and beyond.”
In September Goldschmidt named Steven Falcone, M.D., M.B.A., associate professor of radiology, neurological surgery, and ophthalmology at the Miller School and vice chair of the UM Medical Group, to the post of executive clinical dean for UMMSM@FAU.
A big part of Falcone’s job will be to ensure the regional campus flourishes. It’s well on its way.
One of the most vivid examples can be seen in the quick steps the University has taken to initiate residency training programs. The Internal Medicine Residency Program at UMMSM@FAU recently received approval from the Accreditation Council for Graduate Medical Education to accept its first group of interns in July at its two partner hospitals, JFK Medical Center in Atlantis and the West Palm Beach VA Medical Center.
“This program, which will add primary care and subspecialty physicians to our community, is committed to the highest quality education for our era, emphasizing interdisciplinary patient care, evidence-based medicine, and patient safety,” says Jeannette Mladenovic, M.D., professor of medicine and senior associate dean for graduate medical education.
All the parties to this partnership believe that more medical students and residents will ultimately mean more physicians to address the predicted doctor shortage in Florida.
“The unique partnership between UMMSM and FAU to create a new four-year medical education program is a rapid and cost-effective way to respond to Florida’s physician shortage,” says Michael L. Friedland, M.D., FAU vice president and regional dean for the joint medical program.
What the joint venture has done, says Laurence B. Gardner, M.D., executive dean for education and policy at UM, is “create more places for Florida residents to attend LCME-accredited medical schools by using the physical facilities of the regional campus combined with the intellectual and faculty resources of both UM and FAU. It is residency programs that respond most directly to the critical physician workforce shortage in Florida.”
Satisfying the need for new physicians with ultra-modern technical competencies and real-world, patient relations skills is the cornerstone of the program’s curriculum.
“Thirty-five years ago when I went to medical school we had to memorize basic science. No one said, ‘This is why you have to know this,’” says Lichtstein. “We want students to obtain a deeper form of permanent knowledge that can be utilized when they are seeing and caring for patients.
“These goals and objectives are carefully aligned with the medical campus in Miami,” he stresses. “It’s just that we’re teaching them in a different way.”
While novelty runs throughout the program, one hallmark is the enormous commitment that medical students have as much contact with physicians and patients as possible—starting in the first year and increasing throughout the four years.
For first-year students, each week they form groups of four and spend one afternoon with a faculty member serving patients at a Palm Beach County public health clinic. And for a second afternoon weekly, they are paired with a community preceptor—a physician in private practice—to see patients.
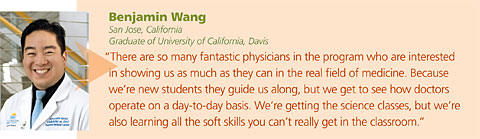
“I had a bunch of choices, but at the end of the day this program was what I was looking for because it stressed learning things outside the classroom,” says Benjamin Wang, who came from San Jose, California.
The way UM educators saw it, a new program of a size that could be more easily managed and monitored was the perfect opportunity to try a more modern approach to teaching.
“If you’re an educator and you get a chance to build a new medical education program from the ground up, you get to build something really innovative,” says Mark O’Connell, M.D., senior associate dean for medical education at UM.
That’s why the forward-thinking curriculum also has an emphasis on the longitudinal management and involvement of the care of patients with chronic diseases. This is an area of medicine that not only lacks enough physicians currently, but the need is expected to grow tremendously as Baby Boomers live longer with chronic ailments.
In light of this, the Association of American Medical Colleges (AAMC) awarded the program a $175,000 grant supported by the Josiah Macy Foundation. According to the AAMC, by 2030 the number of Baby Boomers will double to 71 million. On the other hand, since 1980 the number of first-year medical students per 100,000 persons has declined annually.
“In a given week, every student in the first-year class spends a half-day with a community preceptor and a half-day at the health department clinic,” says Lichtstein. “That means that 20 percent of the curriculum is devoted to patient care. That’s huge.”
Providing care for more patients in Palm Beach County is a goal for the Miller School, and the regional medical campus is the nucleus of this expansion.
Last summer a UM internal medicine practice opened its doors in Palm Beach Gardens. After a decade in that same area, UM’s Bascom Palmer Eye Institute moved into a brand new, technologically advanced eye care center. UM specialty physicians recently set up a practice near the FAU campus, and UM/Sylvester, close by in Deerfield Beach, is a satellite facility of the only university-based cancer center in South Florida.
Eventually, the four-year M.D. program will require even more clinical faculty, an opportunity for UM physicians to operate clinical practices in Palm Beach County while simultaneously preparing new doctors at UMMSM@FAU.
“There are people in Palm Beach County who seek what they perceive to be high-quality health care and, as a result, many go to Boston or Johns Hopkins and other places for complex care,” O’Connell says. “The Palm Beach County leadership sees this need, and UM sees a great opportunity to grow in a place that’s looking for a high-quality, university-based health care system. In this partnership, everyone wins.”
|