Transplanting pancreatic islet cells is a promising treatment option for diabetes, but the therapy presents clinical challenges. Due to insufficient islet cells and their progressive failure over time, insulin independence can be achieved only for a limited time and often requires a second procedure. Physicians seek to improve methods to expand the number of islet cells by making them proliferate more quickly and die more slowly.
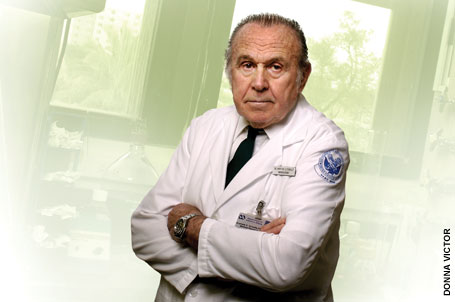 |
| Nobel Prize-winning faculty member Andrew V. Schally, Ph.D., M.D.h.c., D.Sc.h.c., leads an international team of researchers seeking ways to improve methods for pancreatic islet cell transplant. |
An international team of researchers led by the Miller School and the University of Dresden in Germany has discovered a potential method to improve therapeutic results using growth hormone-releasing hormone (GHRH). Andrew V. Schally, Ph.D., M.D.h.c., D.Sc.h.c., the 1977 Nobel Prize winner for Physiology or Medicine, Distinguished Medical Research Scientist of the Department of Veterans Affairs, and Distinguished Professor of Pathology, worked with Norman Block, M.D., professor of pathology, urology, oncology, and biomedical engineering and the L. Austen Weeks Family Professor of Urologic Research, in concert with Stefan Bornstein, M.D., and Barbara Ludwig, M.D., of the Carl Gustav Carus University Hospital in Dresden, and their colleagues in leading the research team, which published its findings online in the June issue of the Proceedings of the National Academy of Sciences.
Pancreatic islets are made up of several types of cells including beta cells, which
are responsible for producing insulin. The research team showed that J1-36, a synthetic agonist of GHRH, caused a significant increase in islet cell proliferation and a reduction in programmed cell death, or apoptosis. Pre-treatment with this particular agonist improved the metabolic function and engraftment of the cells following transplantation. In fact, islets treated with the GHRH agonist before transplantation into diabetic mice were able to produce normal glucose levels in the blood earlier and more consistently than islets without JI-36.
The GHRH agonist, JI-36, in vivo was able to increase cell size leading to in-creased insulin production and quicker insulin production in response to a
glycemic stimulus. “Our hope,” says Schally, “is that, with this discovery, we’ve provided a novel treatment which will improve the management of this disease for millions of patients.” |