While Most cancer cells are identified and eliminated by the immune system, a few may escape this surveillance and spawn tumors and metastases. In the foreseeable future, patients with many forms of cancer could be helped by research led by Eli Gilboa, Ph.D., at the Miller School’s Sylvester Comprehensive Cancer Center.
Gilboa, Dodson Professor of Microbiology and Immunology and co-leader of the Tumor Immunology Program at Sylvester, working with colleagues Fernando Pastor, Ph.D., post-doctoral associate, and Despina Kolonias, M.S., senior research associate, as well as Paloma Giangrande, Ph.D., assistant professor of internal medicine at the University of Iowa, developed an entirely new method to induce the expression of antigens (proteins recognized as foreign by the immune system) on the surface of tumor cells, spurring a much more robust immune response to malignancies. The results of the study, conducted in vitro and with mice, were published in Nature.
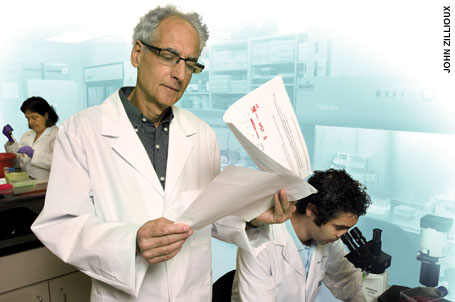 |
| Working with collaborators including Fernando Pastor, Ph.D. (right), Eli Gilboa, Ph.D., has discovered a promising new way to mobilize the body’s immune system to identify and destroy tumor cells. |
Pathogens such as bacteria and viruses express antigens that stimulate an immune-system response. Because tumor cells are similar to normal cells, they don’t express many antigens, thus escaping detection and destruction by the immune system and growing unchecked into cancers. Gilboa’s team devised a method to force tumor cells to express new antigens on their surface, making tumors appear more like pathogens and thus triggering a more potent immune response.
Normally the genetic information encoded in a cell’s DNA is converted to RNA, which then is translated into a protein. During RNA synthesis, a process known as nonsense-mediated mRNA decay detects and eliminates defective RNAs. However, if the nonsense-mediated mRNA process is not functional, the defective RNAs will generate aberrant proteins, which will stimulate an immune response. With this in mind, Gilboa and his team focused on inhibiting the RNA degradation process, but only in tumor cells.
Miller School Dean Pascal J. Goldschmidt, M.D., hailed the research for its potential to offer “a brand new opportunity for the millions of patients who are victims of cancers.”
Gilboa describes his team’s findings as “a potentially significant discovery toward a new therapy” that “could become an alternative to vaccines—simpler, broadly applicable, and potentially more effective.” The next step, he says, would be clinical trials at the Sylvester Comprehensive Cancer Center, with a likely initial focus on cancers such as prostate cancer and/or HER2-positive breast cancer. |